Articles Biceps Tendon Injuries
Biceps tendon injuries are a common source of shoulder pain. Please continue reading to gain a better understanding of these injuries, common symptoms, risk factors and physiotherapy management.
Basic Anatomy
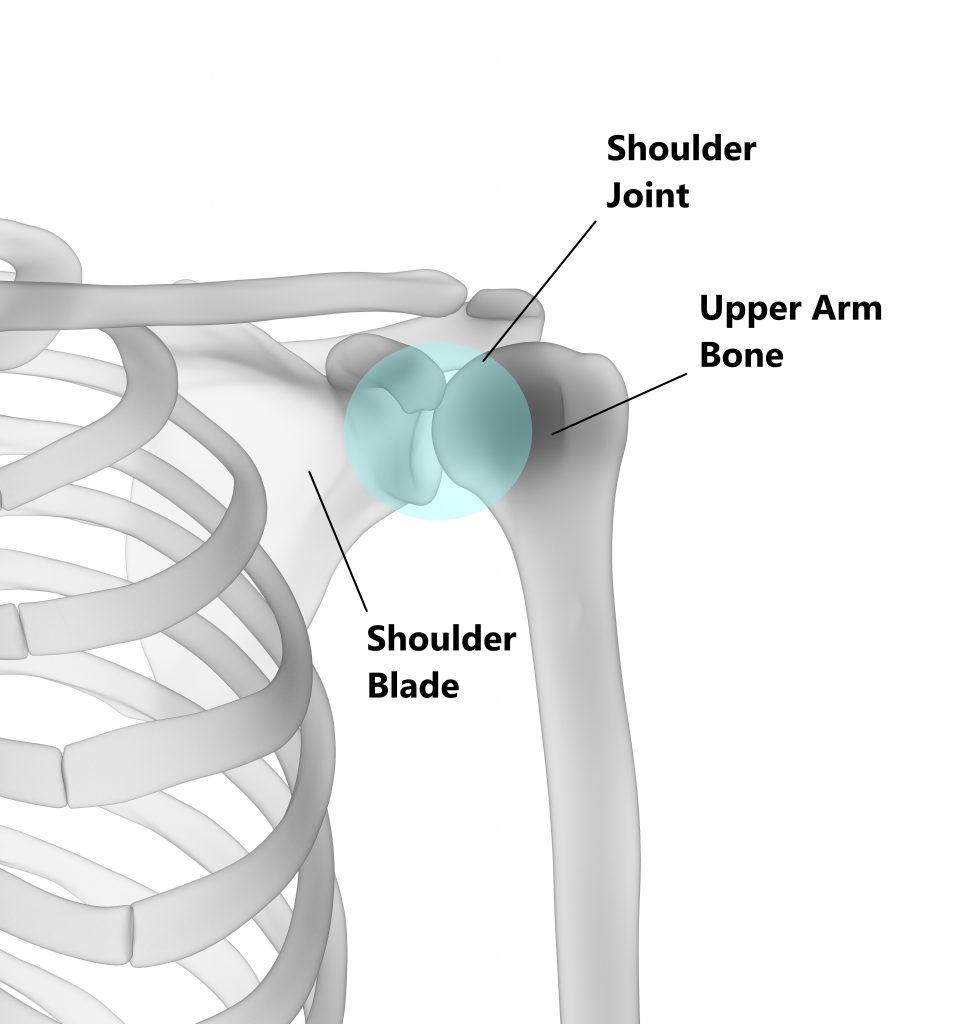
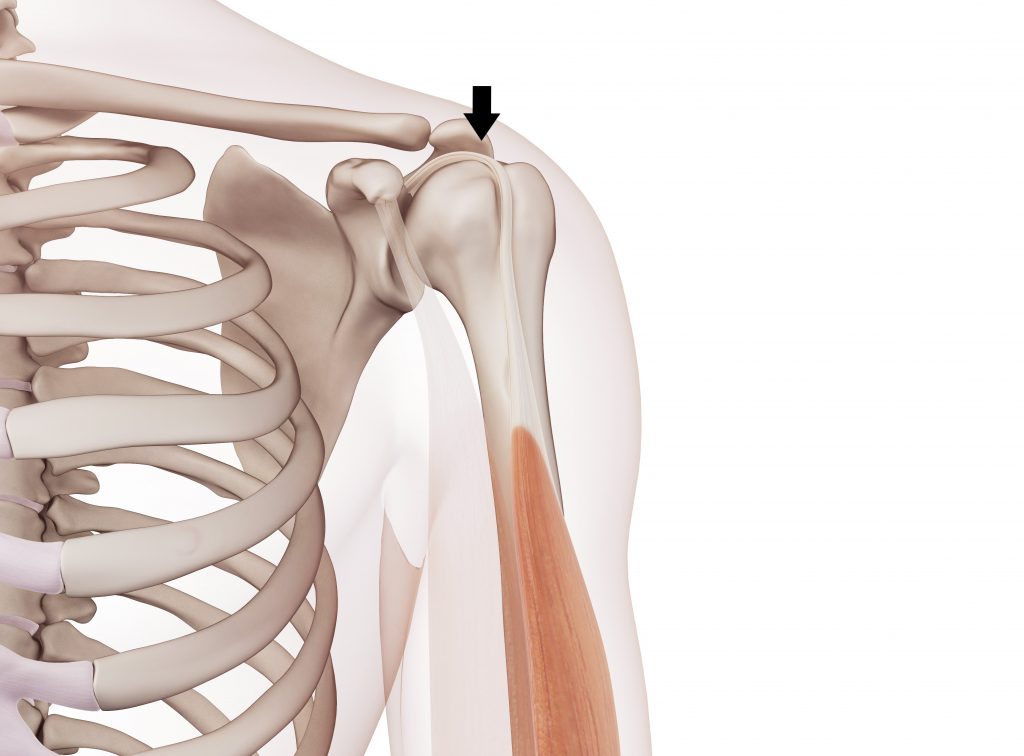
The ball of your upper arm bone connects to the socket of your shoulder blade to form the shoulder joint. This is very much like a golf ball sitting on a tee.
Attached to the front of your upper arm bone is the belly of your biceps muscle.

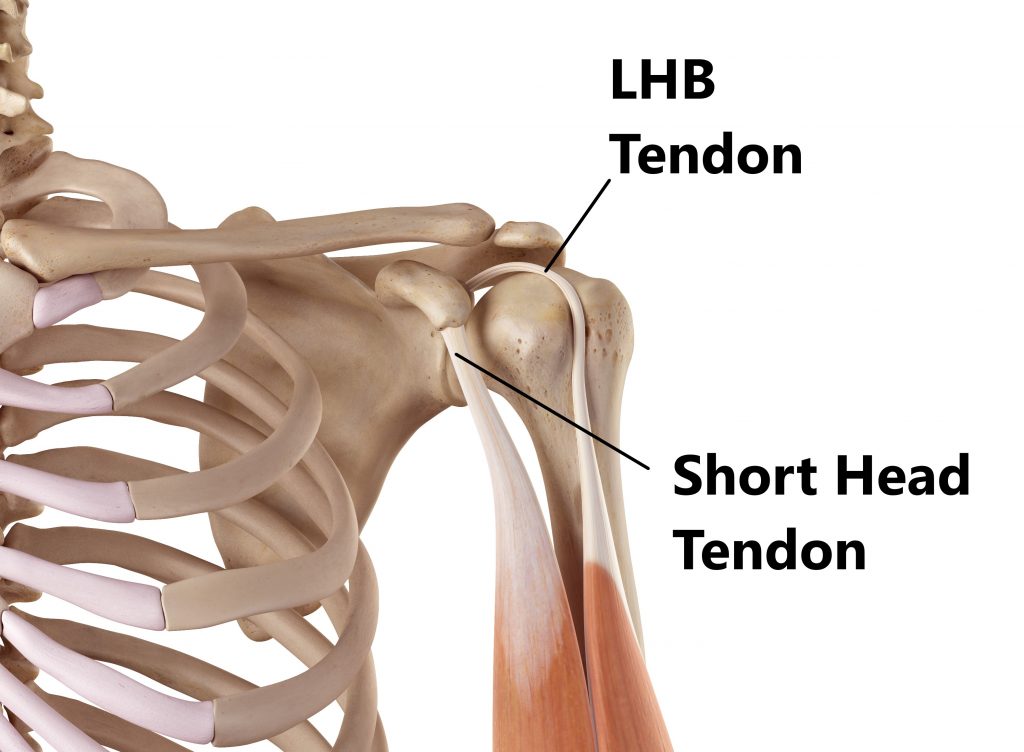
Connecting the muscle to the shoulder blade above we have 2 tendons:
- the long head of biceps (LHB) tendon attaches to the top part of the socket inside the shoulder joint
- the short head of biceps tendon attaches to a bony lump on the shoulder blade outside the shoulder joint
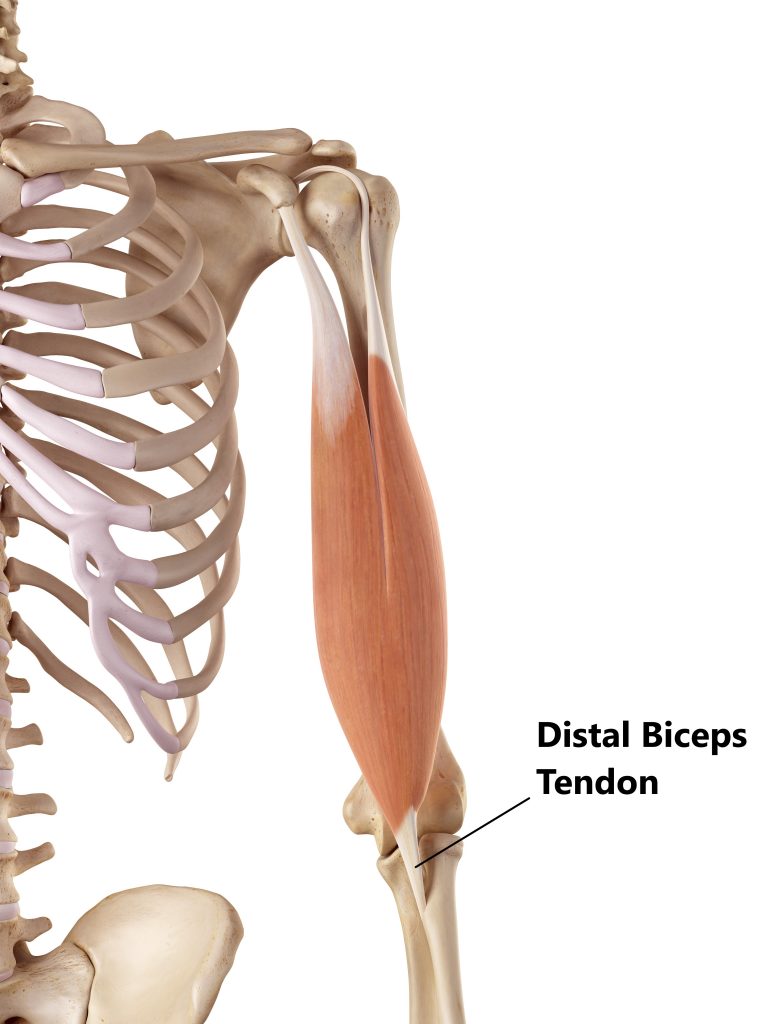
Connecting the muscle to the lower arm bone below we have 1 tendon:
- the distal biceps tendon attaches onto the radius bone near the elbow
What Does the Biceps Muscle Do?
At the elbow your biceps muscle helps to bend the elbow and turn your hand in a “palm up” position.
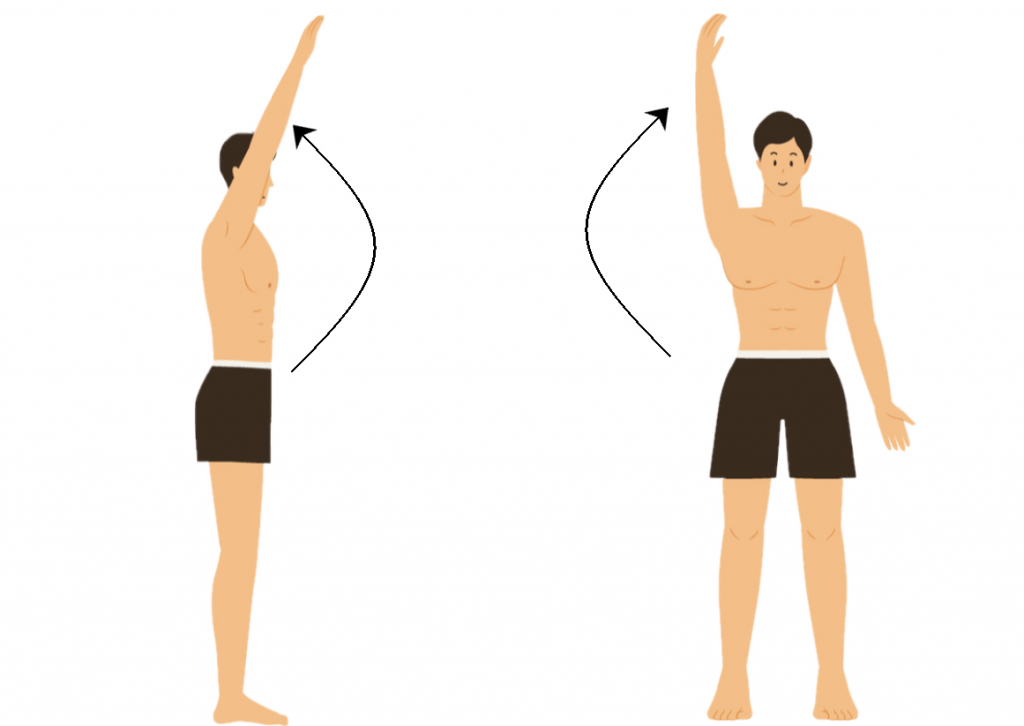
At the shoulder your biceps muscle helps to lift the arm up and away from the body.
The LHB tendon helps to keep the “golf ball”centred on the “tee” during movement by resisting upwards translation.
Biceps Tendon Injuries
Approximately 96% of all biceps injuries involve the LHB tendon. This is because it attaches inside the shoulder joint and is connected to other structures (i.e. ligaments and tendons). Distal tendon injures account for approximately 3% and short head injuries only 1%. We have compiled a list of common injuries below.
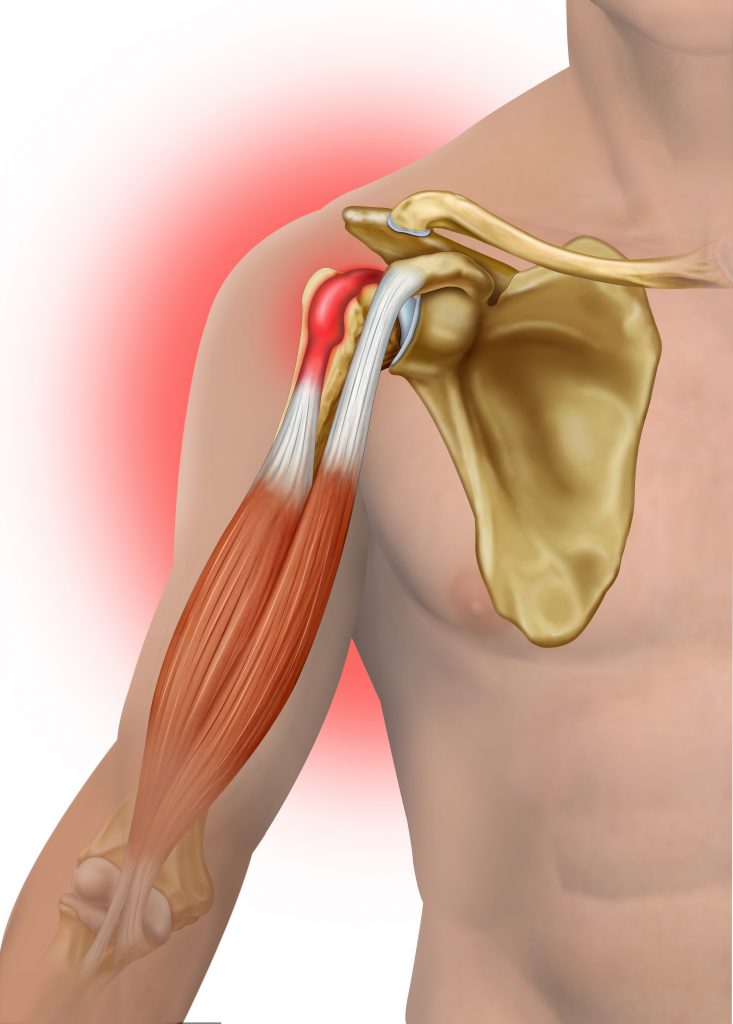
Tendinitis
The LHB tendon can become inflamed and painful following acute trauma (i.e. fall onto an outstretched arm) or from overuse (i.e. repeated overhead activity). Inflammation can also occur in the sheath that surrounds the LHB tendon, this is know as bicipital tenosynovitis.
Tendinitis can also affect in the distal tendon but these injuries normally arise following incidences where the elbow is suddenly or repeatedly bent or straightened against resistance (i.e. repeatedly picking up buckets of sand).
Tendinitis is typically managed conservatively, occasionally a cortisone injection may be required to alleviate inflammation.
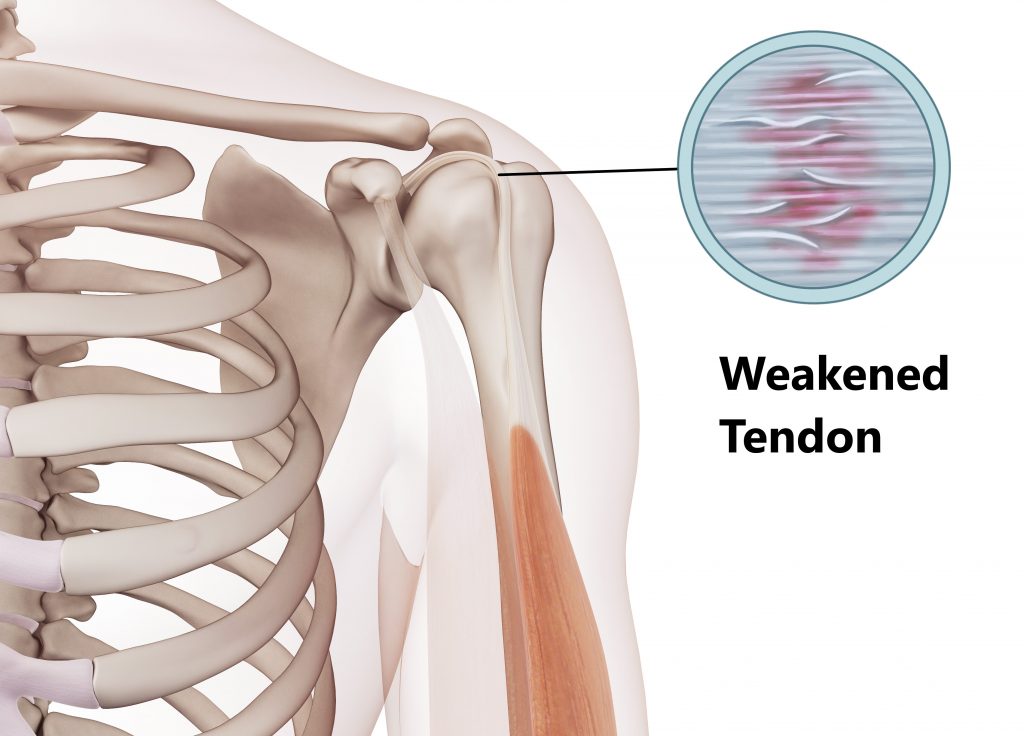
Tendinosis
This is most commonly seen in people from middle age and on wards, it is the result of overuse and natural wear and tear. Tendinosis is characterised by thinning and weakening of the tendon making you more prone to developing tears.
This condition lacks of the presence of inflammation therefore, does not respond well to anti-inflammatory medications. These injuries are best managed conservatively.
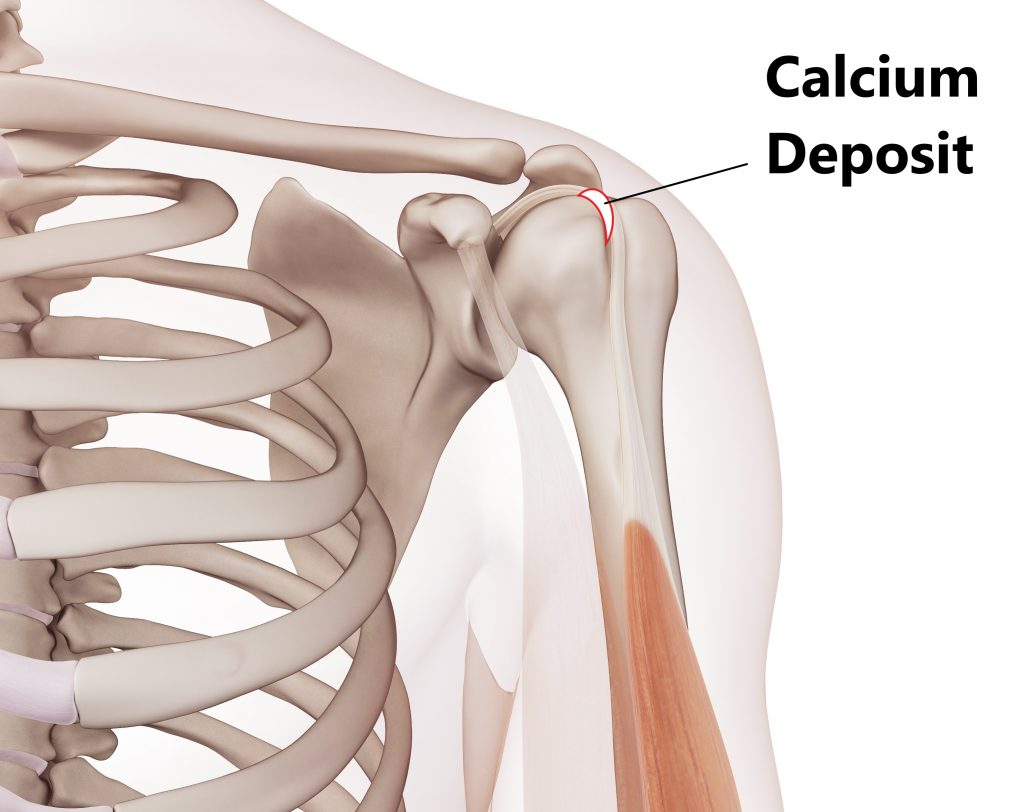
Calcific Tendinitis
This condition is characterised by calcium deposits forming inside the tendons. It is unclear why this occurs but is more often seen in diabetics and in people from middle age and on wards. In most cases the body will reabsorb the calcium deposits. Occasionally non conservative procedures are required to reduce/remove the deposits such as needle aspiration, ultrasound therapy and arthroscopic surgical removal.
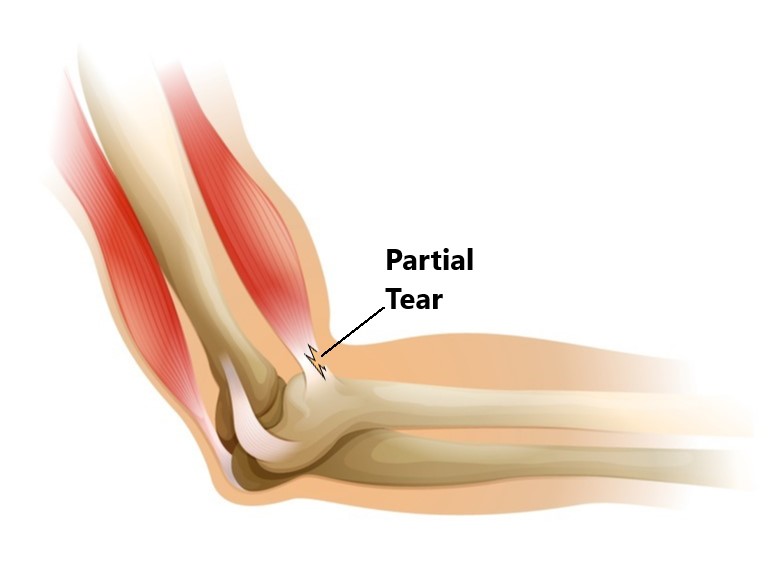
Partial Tendon Tears
Acute Tears, are generally the result of sudden trauma. Small to moderate sized tears are best managed with conservative treatment, occasionally a cortisone injection may be required to alleviate inflammation. Larger tears may require surgical repair.
Degenerative Tears, are more common amongst the general population and a normal part of the ageing process. These are generally due to wear and tear and overuse. As we age the blood supply to our tendons lessen making it easier to develop tears. Degenerative tears do not necessarily require treatment unless the individual is symptomatic.
Complete Tendon Ruptures
Complete tendon ruptures are normally the result of acute trauma where the elbow is bent against heavy resistance (i.e. lifting heavy weights) or where the elbow is suddenly straightened against resistance (i.e. slipping over whilst holding on to a handrail).
We typically see these injures in the dominant arm of males (40-60 years of age) who participate in heavy physical activity (i.e. overhead sports, physical occupations). Individuals often feel a popping sensation at the time of injury. A visible deformity may also be present due to retraction of the muscle fibres (see images below).
Surgery is not always indicated in these situations. The other muscles surrounding the shoulder and elbow joint can compensate to still enable a good level of function. However, if you decide not to have surgery you may be left with a cosmetic deformity, a slight decrease in power and cramping in the biceps muscle. It is always best to have an orthopaedic opinion in these situations to assess your options.
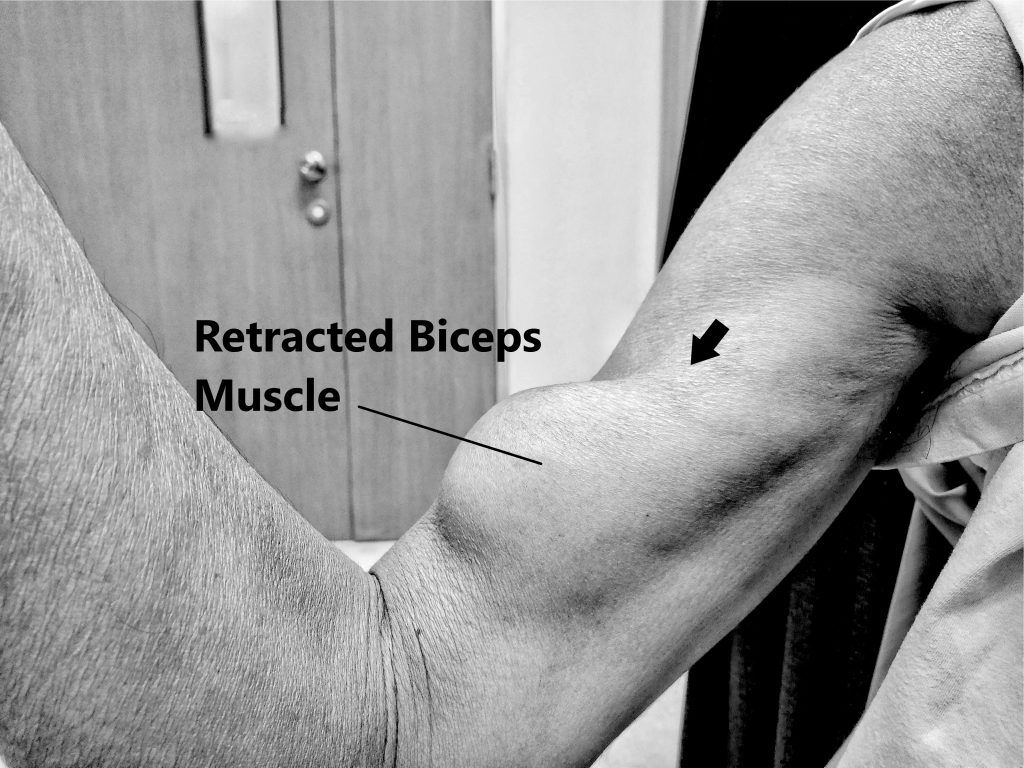
Complete rupture of LHB tendon, muscle fibres retract downwards
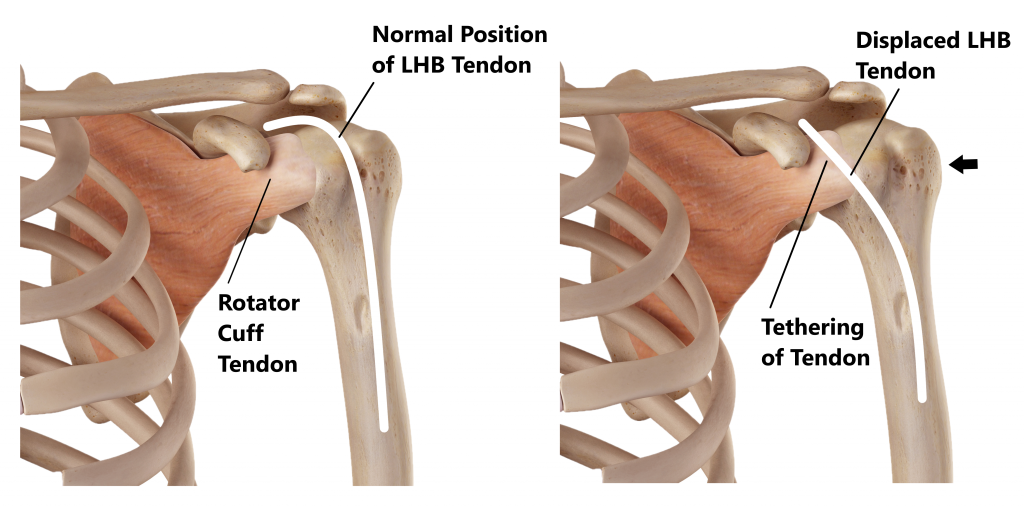
Subluxed LHB
As the LHB tendon travels upwards towards the shoulder joint it normally sits inside a bony groove on the upper arm bone. Damage to the surrounding structures can occur if the LHB tendon becomes displaced out of its groove. This can be due to acute trauma or overuse. Surgery is often required in these situations as the displaced LHB tendon can tether and tear the underlying rotator cuff tendon.
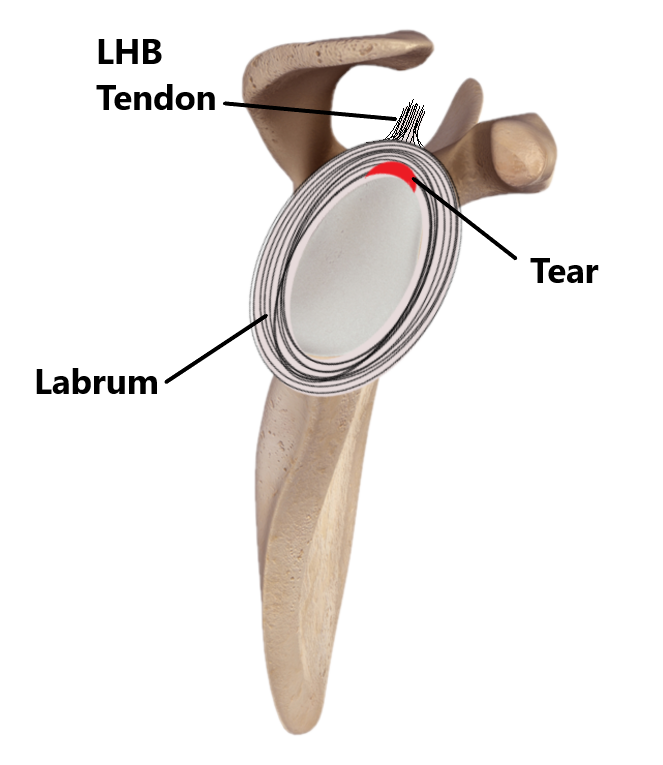
Labral Tear
Surrounding the rim of the socket of the shoulder joint is a ring of cartilage called the labrum. Tearing and detachment of the top part of the labrum along with the LHB tendon can occur from acute trauma (i.e shoudler dislocation) and overuse (i.e repeated overhead activity). Overuse injuries are very common in people who engage in throwing sports (i.e. baseball). Labral injuries are often associated with the feeling of instability and may require surgical repair.
Risk Factors for Biceps Tendon Injuries
- People who are < 40 years of age
- People who engage in occupations and sports involving repeated and prolonged over head activity (i.e. Painters, Volley ball players)
- History of previous shoulder trauma (i.e dislocation, fracture)
- Diabetics

Symptoms of a Biceps Tendon Injury
- weakness
- difficulty lifting the arm for overhead tasks (i.e. hanging up washing)
- pain towards the front of the shoulder, upper arm and elbow
- pain when elevating the arm above shoulder height
- pain lifting the arm away from your body
- pain bending the elbow against resistance
- pain turning your hand in a palm up position against resistance

Other Common Associated Injuries
- subacromial impingement
- shoulder bursitis
- rotator cuff injury
- labral injury
- osteoarthritis of the glenohumeral joint
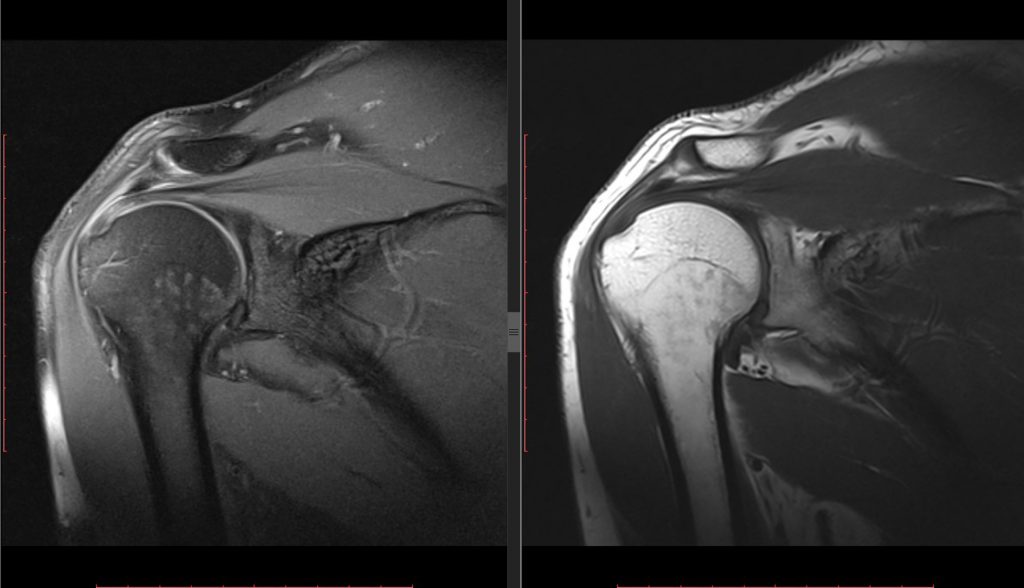
Diagnosis
Diagnosing a biceps tendon injury is based on an individuals clinical presentation and imaging. In many cases imaging is not always necessary.
- Subjective and Physical Examination
- Xray
- Ultrasound
- MRI
Physiotherapy Management
- Following an acute injury our priority is to minimise the extent of damage, reduce inflammation and decrease pain. Modalities such as RICE (Rest, Ice, Compression, Elevation), strapping, manual therapy and acupuncture may also be used.
- Provide education, address unhelpful beliefs regarding the injury, identify and modify aggravating factors
- Restore pain free shoulder and elbow range of motion and prevent secondary complications (i.e. development of a frozen shoulder). Commence movement and stretching exercises.
- Strengthen the rotator cuff and muscles surrounding the shoulder blades. Commence a graded strengthening program.
- Identify and address movement and postural issues that may have contributed to the injury (i.e. stooped posture, poor positioning of the shoulder blades, lack of spine/hip mobility).
- Graded return to work, sport and function.
Please keep in mind the information provided is general in nature and should not be used as a substitute to consult your treating health professional. If you have any specific questions or require assistance with your individual treatment requirements please do not hesitate to contact My Family Physio Mona Vale, inside My Health Medical Centre.
Related Articles