Articles Modic Changes
Modic changes can give rise to neck and back pain and are related to spinal degeneration. Please continue reading to gain a better understanding of this condition, causes, risk factors and management.
Basic Anatomy
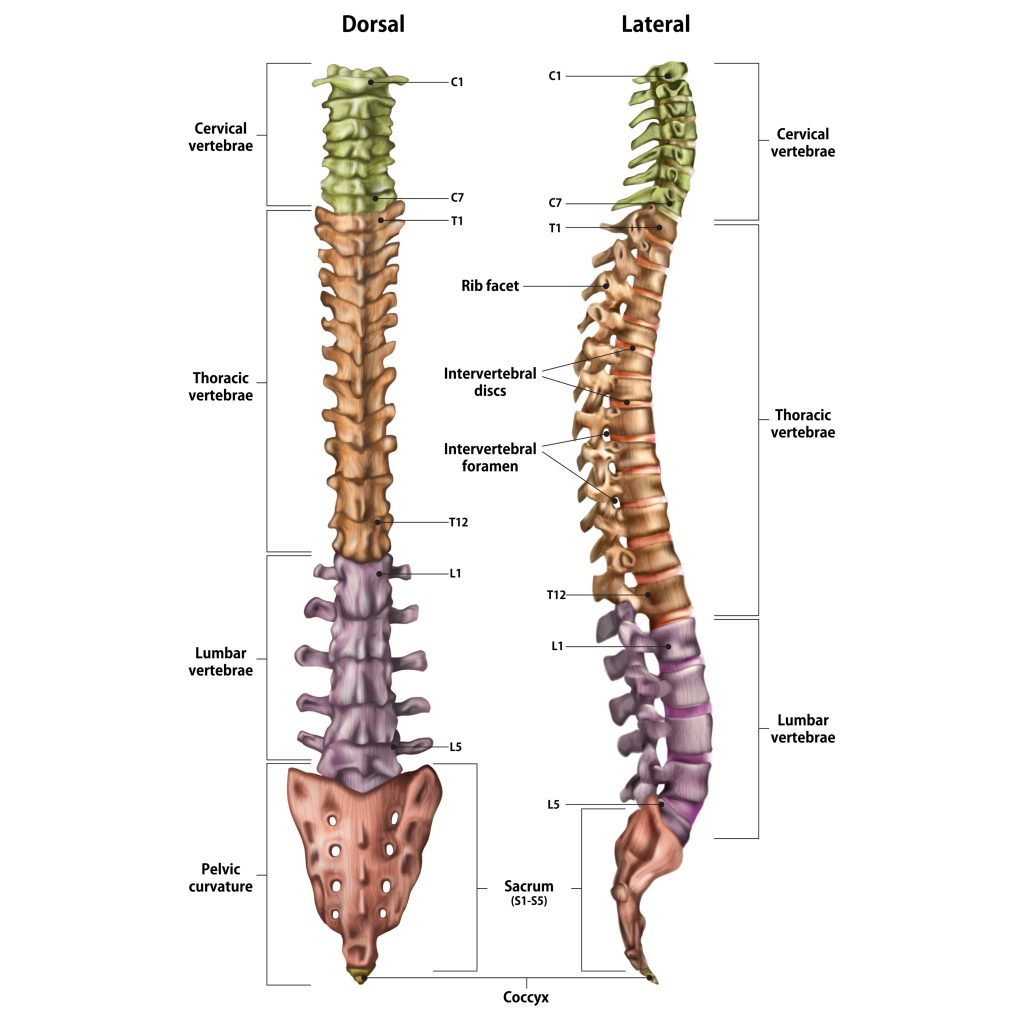
Your spinal column is made up of individual bones called vertebrae and named accordingly to their position in the spine (see below). Your spine is divided into 4 sections:
- Cervical spine (neck) C1-C7
- Thoracic spine (upper back) T1-12
- Lumbar spine (lower back) L1-5
- Sacrum (pelvic area) S1
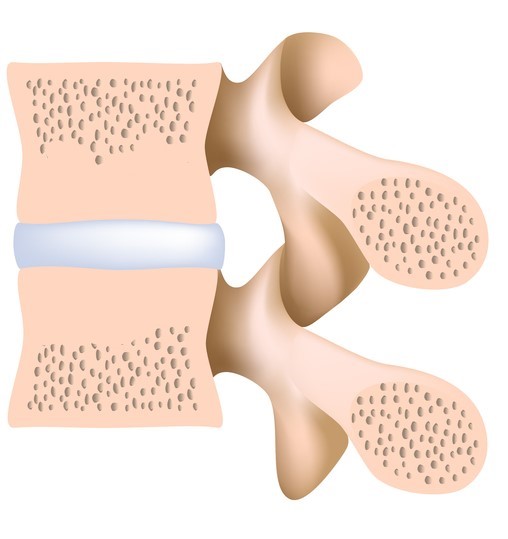
Each Vertebae has 2 layers of bone:
- a dense thicker out layer called “compact bone”
- a porous inner layer called “spongy bone”
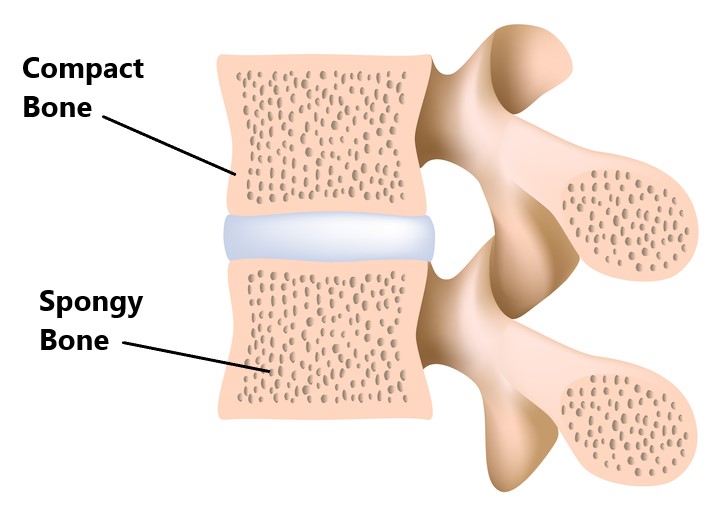
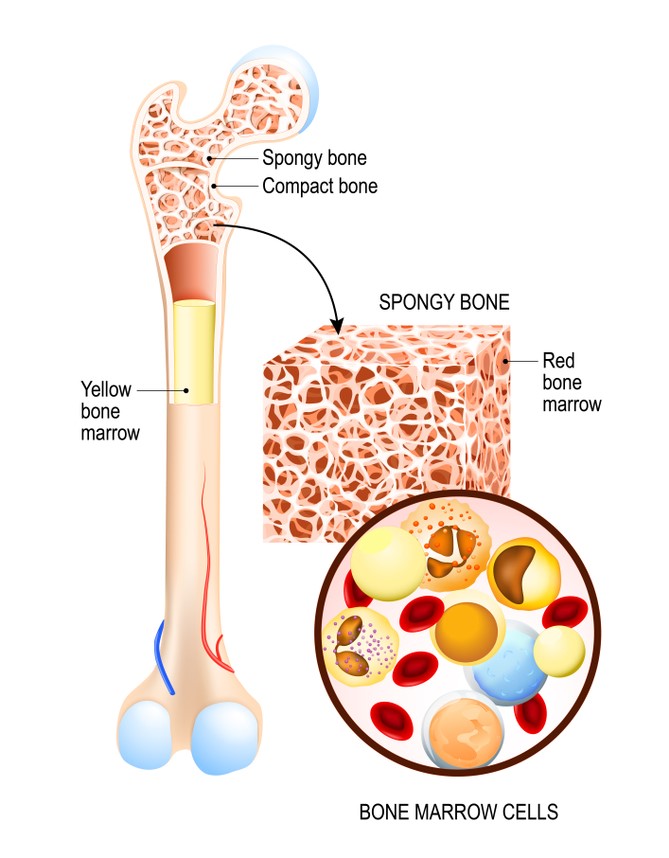
The spongy bone houses your bone marrow which is responsible for making blood cells (red bone marrow) and storing fats (yellow bone marrow).
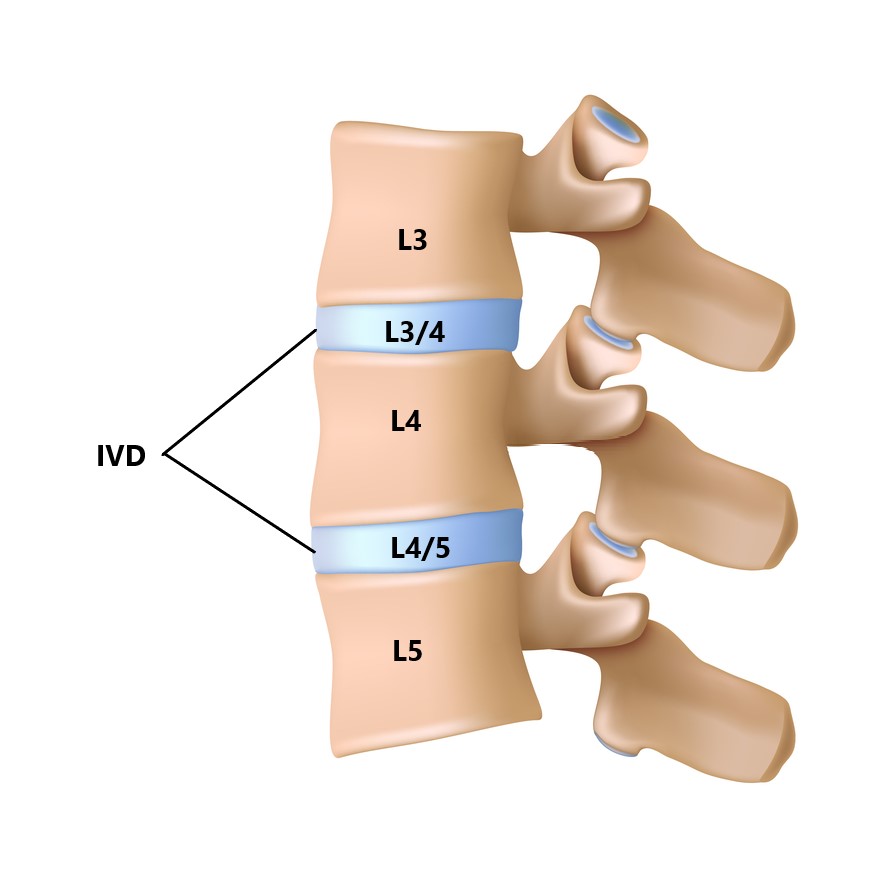
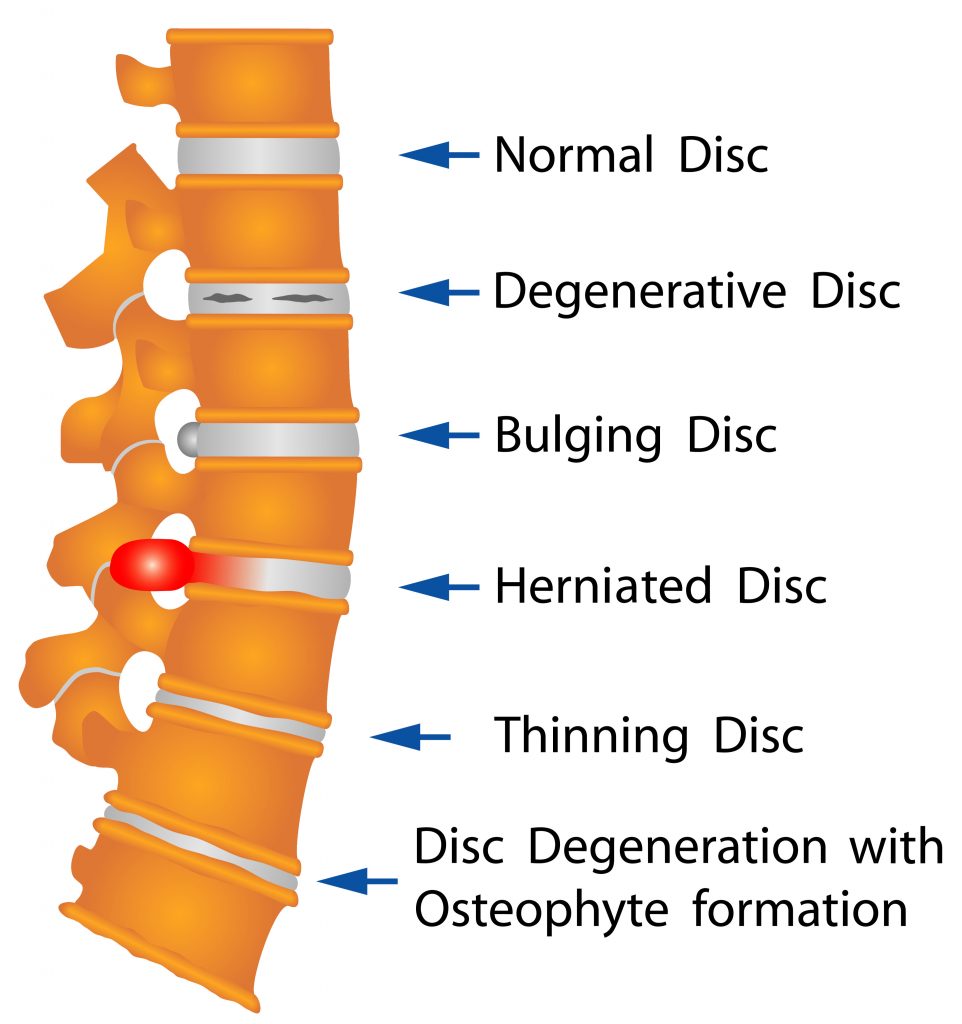
Between each vertebrae is an intervertebral disc (IVD). Each IVD is named relative to the vertebrae they sit between (see below ).
What Are Modic Changes?
Modic changes refer to breakdown of the compact bone and marrow which surrounds the IVD. This is related to spinal degeneration and can be divided into 3 types:
Type 1: characterised by swelling and acute inflammation of the bone marrow
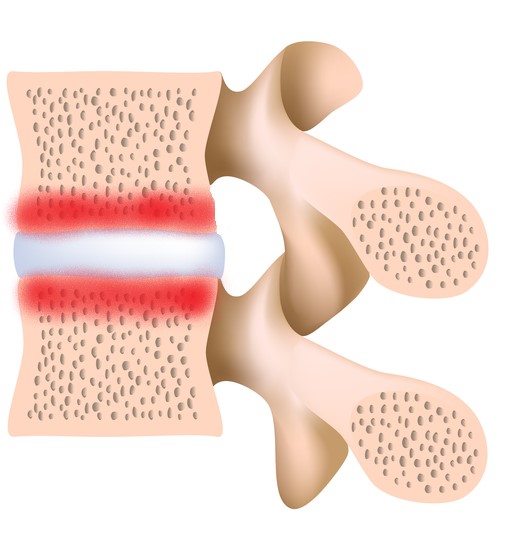
Type 2: characterised by replacement of the red marrow with fatty yellow marrow
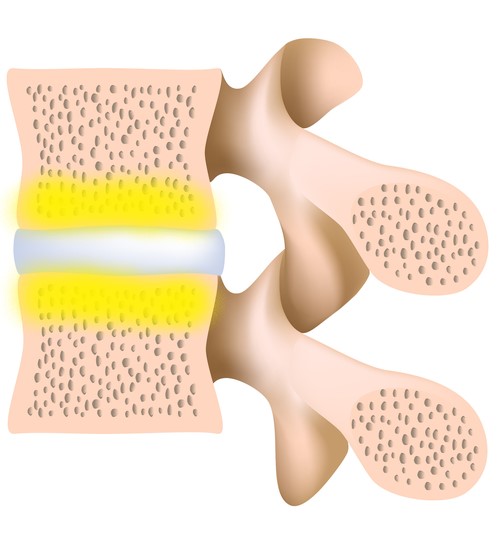
Type 3: characterised by hardening and thickening of the spongy bone, reducing the amount of bone marrow
These can be viewed as different stages of the same disease process. Each stage can potentially progress (i.e. Type 1 to Type 2) or regress (i.e. Type 1 to normal) over an extended period of time (>12 months).
Modic changes can affect all areas of the spine but are most commonly seen in the neck (C5/6) and lower back (L4/5, L5/S1). This condition rarely occurs in isolation and is normally associated with an injury to the IVD (i.e. disc bulge/prolapse).
Due to the presence of acute inflammation, Type 1 changes reflect the first stages of spinal degeneration and are normally associated with pain. Types 2 and 3 lack the presence of acute inflammation therefore, do not typically give rise to symptoms. Type 1 changes have been found to occur in up to 4% of people who have LBP.
What Causes Type 1 Modic Changes?
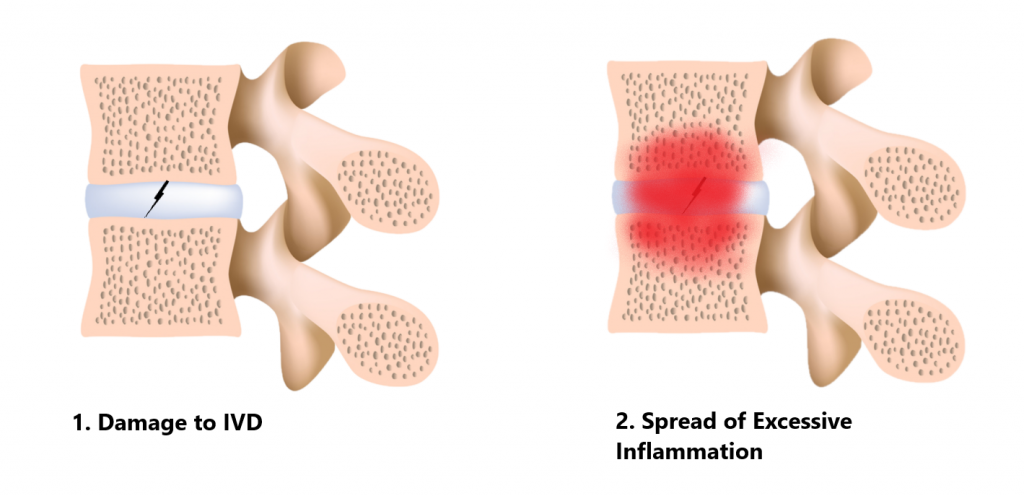
Unfortunately, the causes of Modic changes are still not very well understood. What the researches do agree on however, is the process involves damage to the IVD and the presence of excessive inflammation.
Some researchers believe repeated trauma to the IVD and surrounding bone will eventually give rise to excessive inflammation which travels through to the neighbouring vertebrae (see image below).
Other researches believe trauma to the IVD enables entry of harmful bacteria giving rise to inflammation. Interestingly, this finding made headlines worldwide claiming back pain could be treated with antibiotics. Unfortunately, the circumstances surrounding these studies were controversial and subsequent research has failed to support these findings.
Common Symptoms
- constant pain
- pain at night
- significant activity limitation
- minimal improvement in symptoms after 4-6 weeks following initial injury
- localised back pain +/- referred pain in to the arms or legs
PLEASE NOTE: Constant pain which is also present at night can be indicative of malignancy, please seek URGENT medical attention if you have this symptom!!!

Risk Factors
- smoking
- high BMI
- previous damage or surgery to the IVD
- physically demanding occupations
- older age

Common Associated Injuries
- nerve and spinal cord irritations
- IVD injuries
- facet joint injuries
Diagnosis
It can be difficult to accurately diagnose this condition from a subjective and physical examination, an MRI scan will be required. Other forms of imaging typically used to investigate spinal pain (i.e. xray, CT) will not detect Modic changes but will be useful in ruling out other causes.

Management
Type 1 changes are typically managed with conservative physiotherapy treatment. In some instances an IVD cortisone injection maybe required to help alleviate inflammation. Surgical intervention is not indicated in treating this condition.

Physiotherapy Management
- Our priority is to minimise the extent of damage, reduce inflammation and decrease pain. Modalities such as strapping, manual therapy, hydrotherapy and acupuncture may be used
- Provide education regarding the injury, address unhelpful beliefs, identify and modify aggravating factors
- Restore pain free range of motion and return to basic activities.
- Restore strength of the core and lower limbs.
- Identify and address movement and postural issues which may have contributed to the injury.
- Graded return to work, sport and function.

Red Flags!
These are signs and symptoms of more serious causes and require urgent medical review:
- spinal cord signs (i.e. bladder and bowel weakness, sexual dysfunction, bilateral upper or lower limb weakness or clumsiness)
- symptoms are also associated with a lack of balance and changes in gait pattern
- onset of symptoms following trauma (i.e. fall, car accident)
- constant symptoms and night pain (as discussed above)

Please keep in mind the information provided is general in nature and should not be used as a substitute to consult your treating health professional. If you have any specific questions or require assistance with your individual treatment requirements please do not hesitate to contact MyFamily Physio Mona Vale, Northern Beaches Sydney.
Related Articles