Articles Frozen Shoulder
This article explains what a frozen shoulder is, symptoms, causes, risk factors, diagnosis, medical and physiotherapy management.
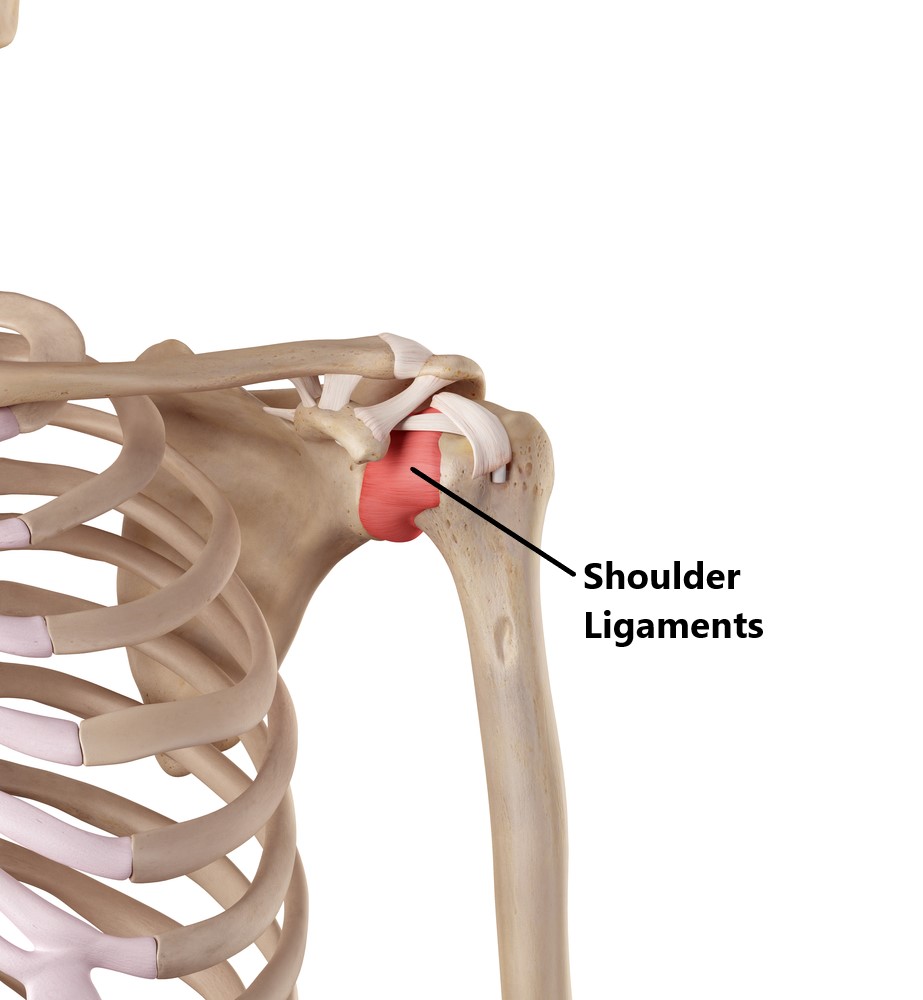
Basic Anatomy
The ball of your upper arm bone connects to the socket of your shoulder blade to form the shoulder joint.
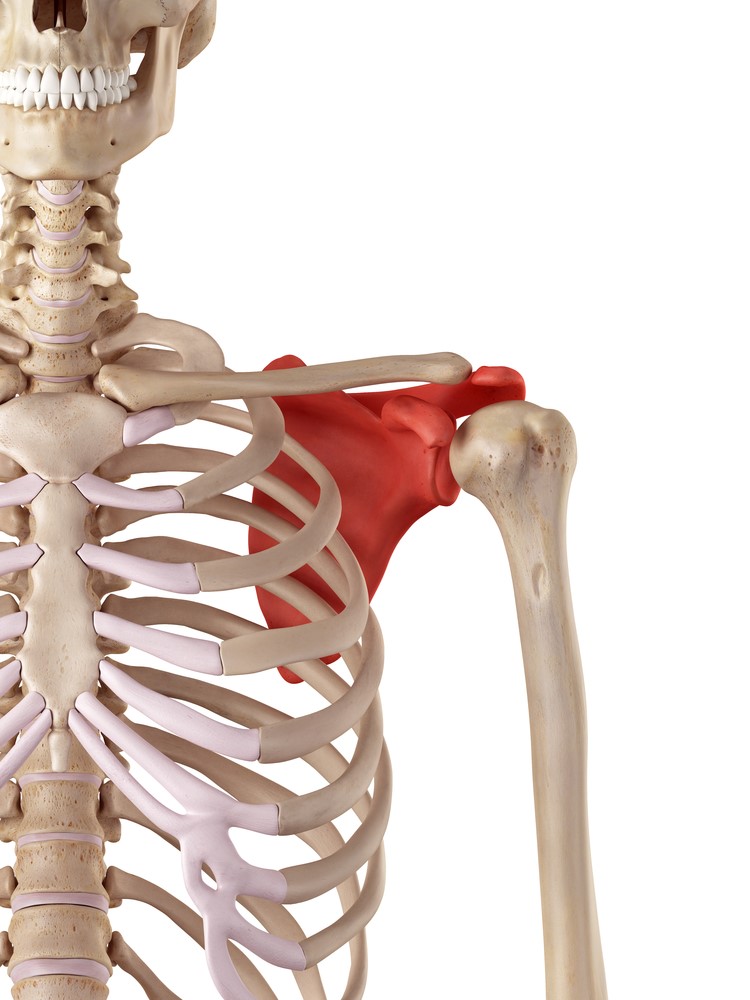
Connecting the ball to the socket is a strong ligamentous joint capsule.
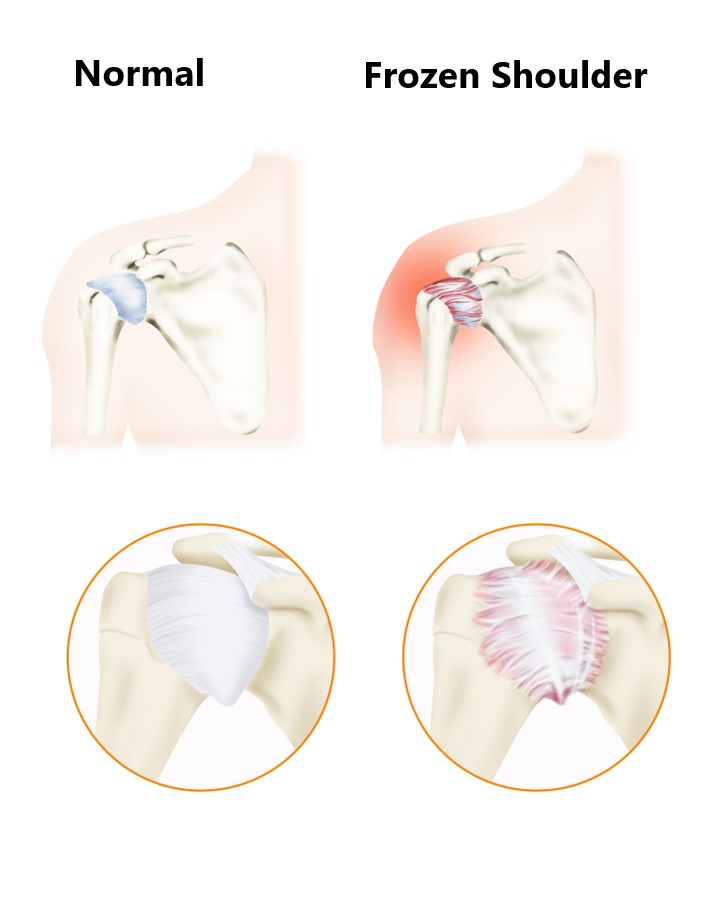
What is a Frozen Shoulder (aka Adhesive Capsulitis)?
A frozen shoulder is caused by shortening and stiffening of the joint capsule, this results in pain and a restriction of shoulder movement in all directions. Researches don’t quite fully understand why this occurs but many believe it is triggered by inflammation inside the joint capsule.
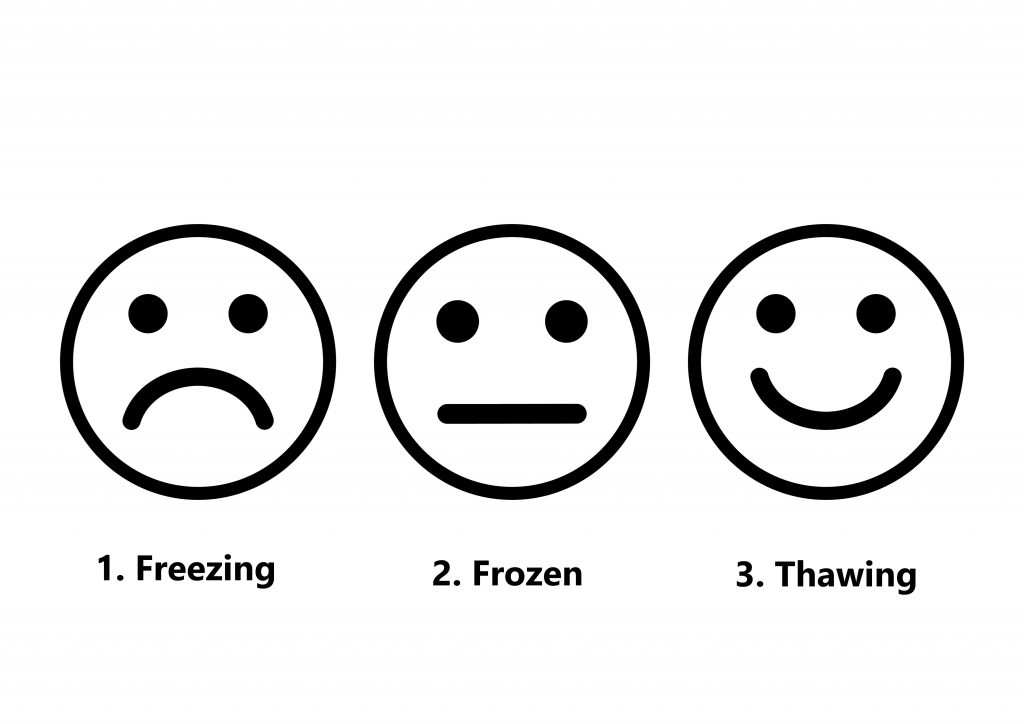
This condition involves 3 overlapping stages:
- Stage 1 Freezing Phase, characterised by increasing pain and a progressive deterioration in movement
- Stage 2 Frozen Phase, characterised by an improvement of pain and marked joint stiffness in all directions
- Stage 3 Thawing Phase, characterised by a gradual improvement in joint stiffness and shoulder movement
Unfortunately, frozen shoulders typically take a long time to heal. Recovery times vary greatly between individuals (i.e. 6 – >24 months). The good news is this condition will gradually resolve itself and most people will make a full recovery.

What are the Symptoms of a Frozen Shoulder?
- restriction of shoulder movement in ALL directions
- joint stiffness
- shoulder pain (in the early stages)
- difficultly with functional tasks (i.e. reaching behind your back, reaching behind your head)

What Causes a Frozen Shoulder?
Spontaneous Onset
Unfortunately, a frozen shoulder can occur out of the blue with no history of injury or trauma. This is more likely to occur in people who are high risk (see below).

Post Trauma
Trauma to the structures inside and surrounding the shoulder joint (i.e. fractures, rotator cuff tears).

Post Surgery
Surgeries directly (i.e. rotator cuff repair) and indirectly (i.e. cardiothoracic surgery, breast surgery) affecting the shoulder joint .

Prolonged Immobility
Not moving your shoulder for prolonged periods of time (i.e. prolonged use of a shoulder sling).

Risk Factors
- females
- 40-65 years of age
- heart and lung disease
- inflammatory conditions (i.e. rheumatoid arthritis)
- diabetics
- stroke victims
- hypo/hyper thyroidism
- autoimmune disease
- cervical disc degeneration

Diagnosis
Diagnosing this condition is mainly based on an individual’s clinical presentation through a thorough subjective and physical examination. An xray, ultrasound or MRI may also be required to exclude/identify other injuries.

Treatment
Most cases of frozen shoulder will gradually resolve on their own. Depending on what stage your shoulder is at, certain interventions can be beneficial in speeding up the recovery process.
- Conservative physiotherapy treatment is often the preferred treatment option (see below).
- A cortisone injection into the joint capsule can help to reduce inflammation
- A procedure called a hydrodilatation involves stretching out the joint capsule by injecting saline into it. This procedure is not very commonly used and studies have found it to be of only limited benefit.
- Surgery is extremely rare and only reserved for those who have not made a full recovery despite comprehensive physiotherapy treatment. The procedure will normally involve surgically releasing the joint capsule and stretching the shoulder while under anaesthetic.

Physiotherapy Management
- Alleviate symptoms and decrease pain. Modalities such as strapping, massage, manual therapy and acupuncture may be used.
- Provide education, set realistic expectations, identify and modify aggravating factors
- Continually to reassess the shoulder for other injuries.
- Restore pain free shoulder range of motion
- Prevent secondary complications (i.e. neck and upper back pain)
- Strengthen the rotator cuff and muscles surrounding the shoulder blades.

Please keep in mind the information provided is general in nature and should not be used as a substitute to consult your treating health professional. If you have any specific questions or require assistance with your individual treatment requirements please do not hesitate to contact MyFamily Physio in Pittwater Place Shopping Centre in Mona Vale.
Related Articles