Articles Tennis Elbow (Lateral Epicondylitis)
This article covers basic anatomy, what tennis elbow is, symptoms, causes, risk factors, diagnosis, medical and physiotherapy management.
Basic Anatomy
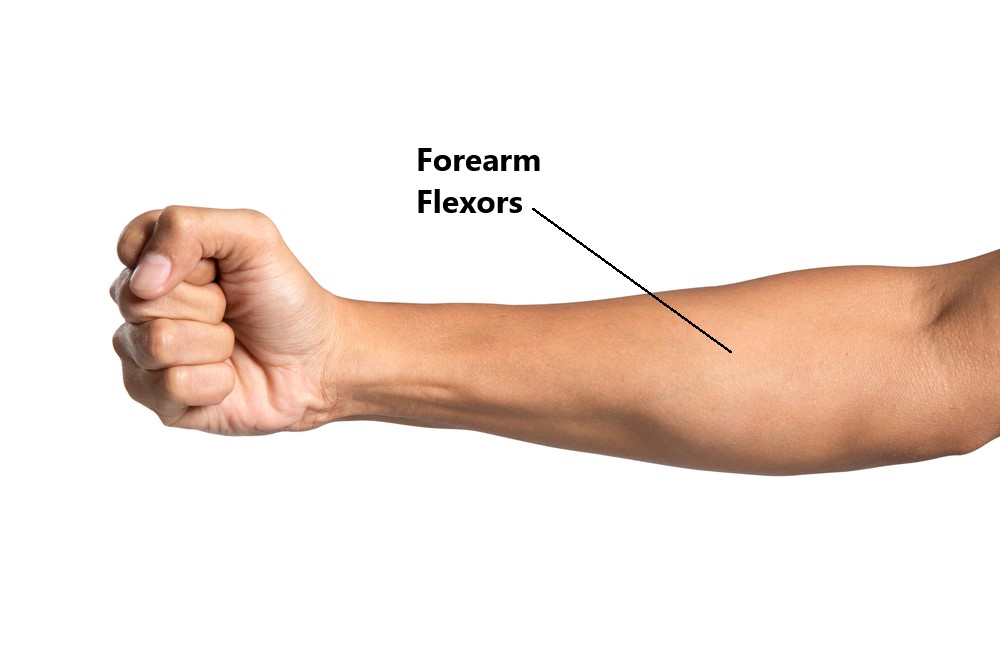
Your forearm has 2 main muscle groups:
- Flexor Forearm Muscles, located on the palm side of your forearm. These muscles are responsible for closing your fingers and bending your wrist.
- Extensor Forearm Muscles, located on the back side of your forearm, These muscles are responsible for extending your fingers and wrist.

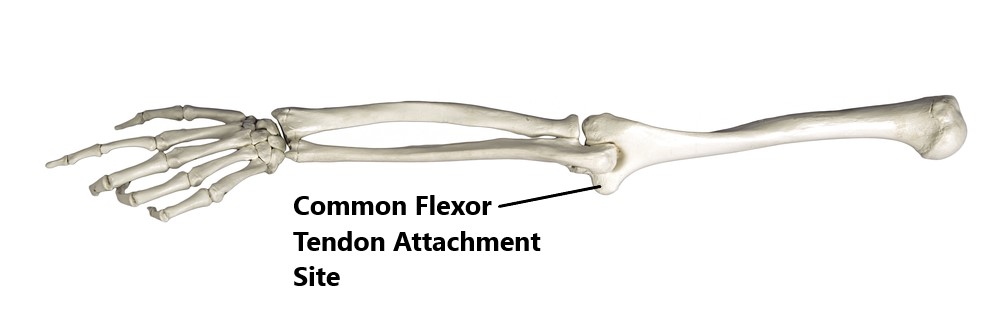
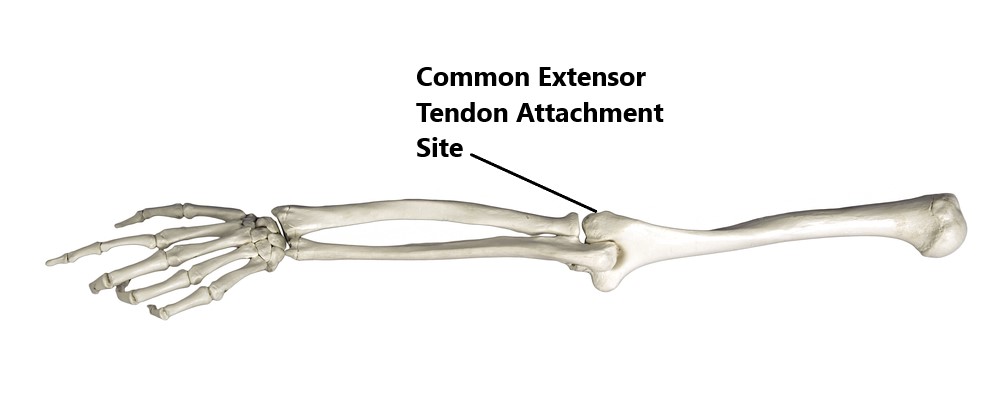
At the elbow joint these muscles attach onto the bone via 2 tendons:
- Common Flexor Tendon, attaching to the inner side of the elbow
- Common Extensor Tendon, attaching to the outer side of the elbow
What is Tennis Elbow (Lateral Epicondilytis)?
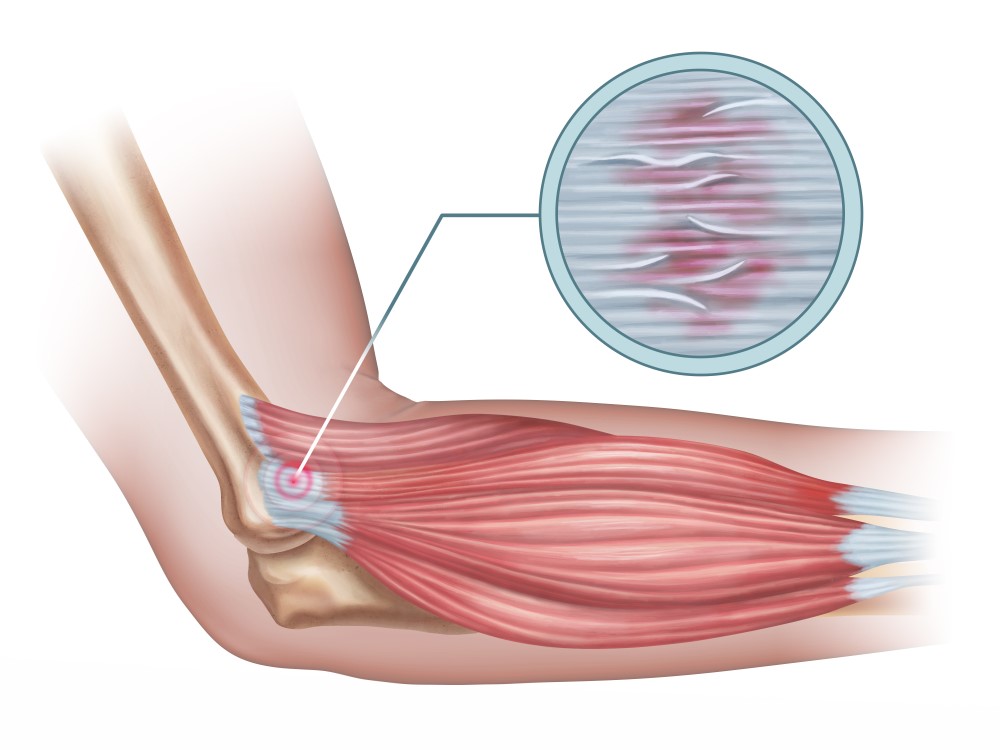
Commonly known as “tennis elbow”, this condition involves pain on the outside of the elbow where the extensor tendon attaches to the bone.

This is very common amongst tennis players however, it can also affect anyone who engages in regular repetitive activity of the hands. This is typically an overuse condition where repeated activity (normally repetitive gripping) results in pain and weakness when trying to grasp objects.

In the early stages (>6 weeks), small microtears in the extensor tendon can lead to inflammation and pain.
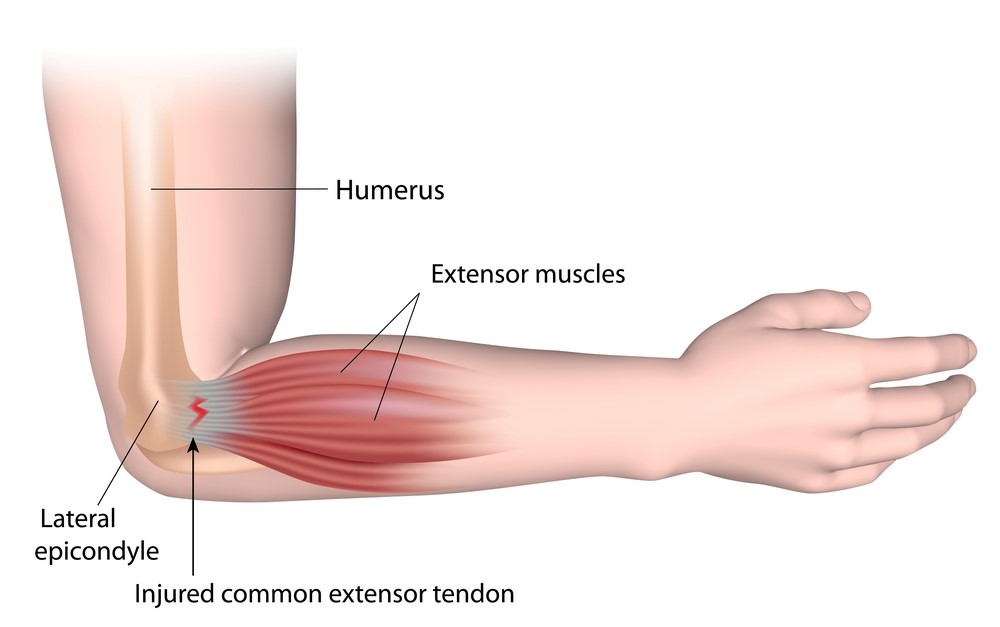
In chronic long standing (> 3 months) cases there is very little inflammation. However, the tendon tissue begins thin and weaken making it easier to develop larger tears. This is why chronic cases do not respond well to anti inflammatory medication ( i.e. Voltaren, cortisone injections)
Common Symptoms
- pain over the outside of the elbow and back of the forearm
- pain and weakness with tasks involving gripping (i.e. using tools) or repeated use of the hands (i.e. typing)
- tenderness and tightness over the back of the forearm and extensor tendon
- pain with making a fist
- difficulty lifting objects (i.e. cup of tea)

Causes
- unaccustomed activity
- incorrect racket set up
- incorrect gripping technique
- over use
- repeated lifting (especially with your palm facing downwards)

Risk Factors
- aged between 30-50 years
- participating in racket sports
- occupations involving repetitive use of the hands (>2 hours per day), tool use and lifting <20 kg
- people with other upper limb problems (i.e. rotator cuff injury, carpal tunnel)
- smokers
- more common in dominant arm

Diagnosis
Diagnosing this condition is mainly based on an individual’s clinical presentation through a thorough subjective and physical examination. An X-Ray, ultrasound or MRI may also be required to assess the severity of the condition and to exclude/identify other injuries.

Management
- most cases will resolve with conservate physiotherapy treatment (see below)
- anti inflammatory medication may be beneficial in the early stages
- occasionally a cortisone injection into the tendon may help to alleviate symptoms
- Plasma Rich Protein (PRP) injections are occasionally used to promote tendon healing however, there is conflicting evidence amongst researches on how beneficial they are
- surgery is rare and only reserved for those who have not made a full recovery despite comprehensive physiotherapy treatment.

Physiotherapy
- Following an acute injury our priority is to minimise the extent of damage, reduce inflammation and decrease pain. Modalities such as modified rest, taping, manual therapy and acupuncture may be used.

- Provide education regarding the injury, address unhelpful beliefs, identify and modify aggravating factors (i.e. lifting objects palm down)

- Restore pain free elbow and wrist range of motion

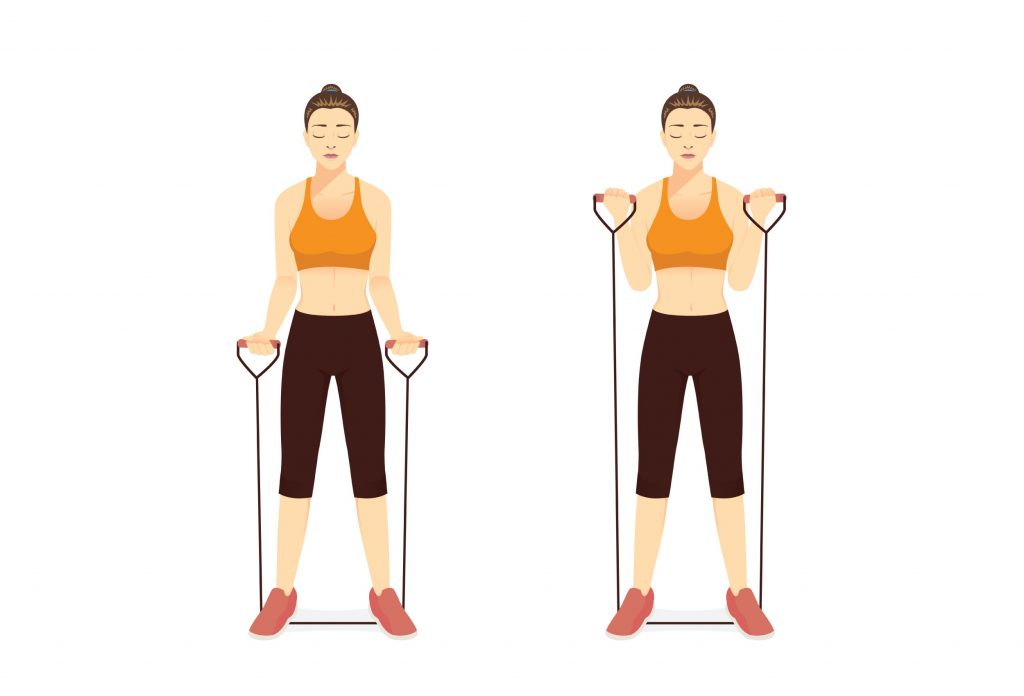
- Restore strength of the muscles of the forearm and shoulder
- Identify movement/postural issues which may have contributed to the injury

Please keep in mind the information provided is general in nature and should not be used as a substitute to consult your treating health professional. If you have any specific questions or require assistance with your individual treatment requirements please do not hesitate to contact MyFamily Physio in Pittwater Place Shopping Centre in Mona Vale.
Related Articles