Articles Baker’s Cyst
This article covers basic anatomy, what a Baker’s cyst is, symptoms, causes, diagnosis, medical and physiotherapy management.
Basic Anatomy
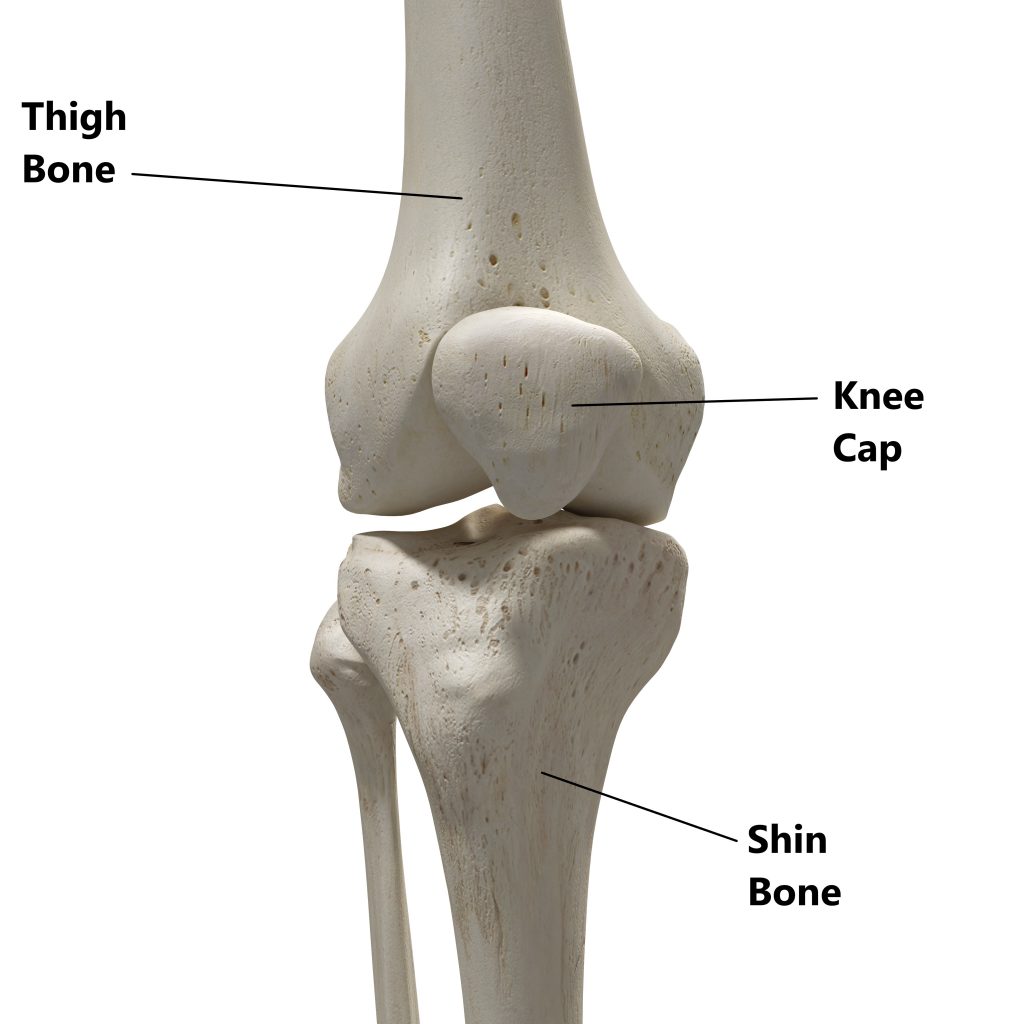
Your knee joint is comprised of 3 bones.
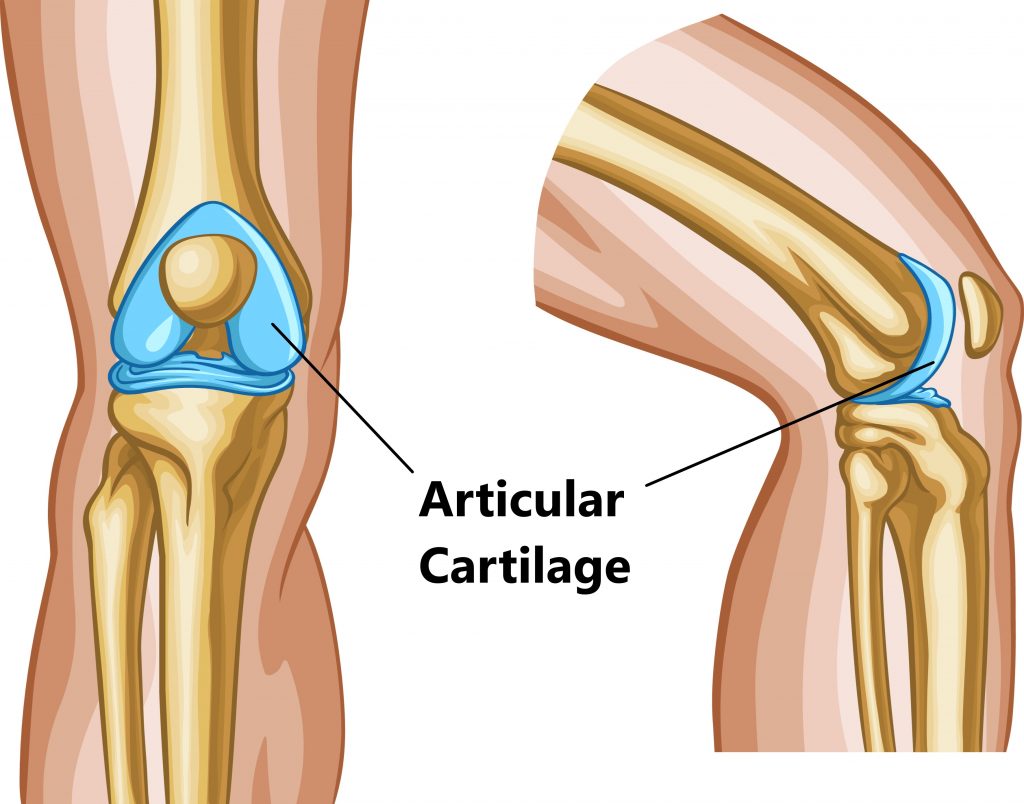
Lining the articulating surfaces is joint cartilage, this allows smooth frictionless movement.
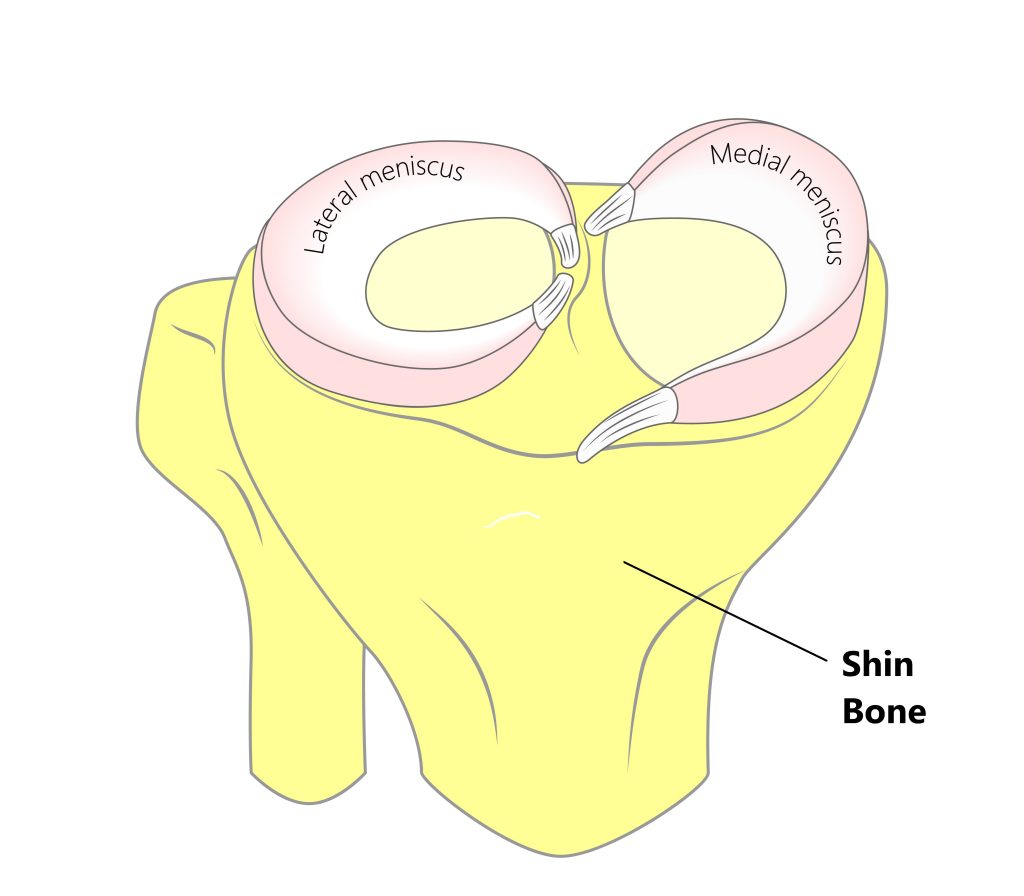
Acting as shock absorbers you have 2 pads of strong fibrocartilage called the meniscus.
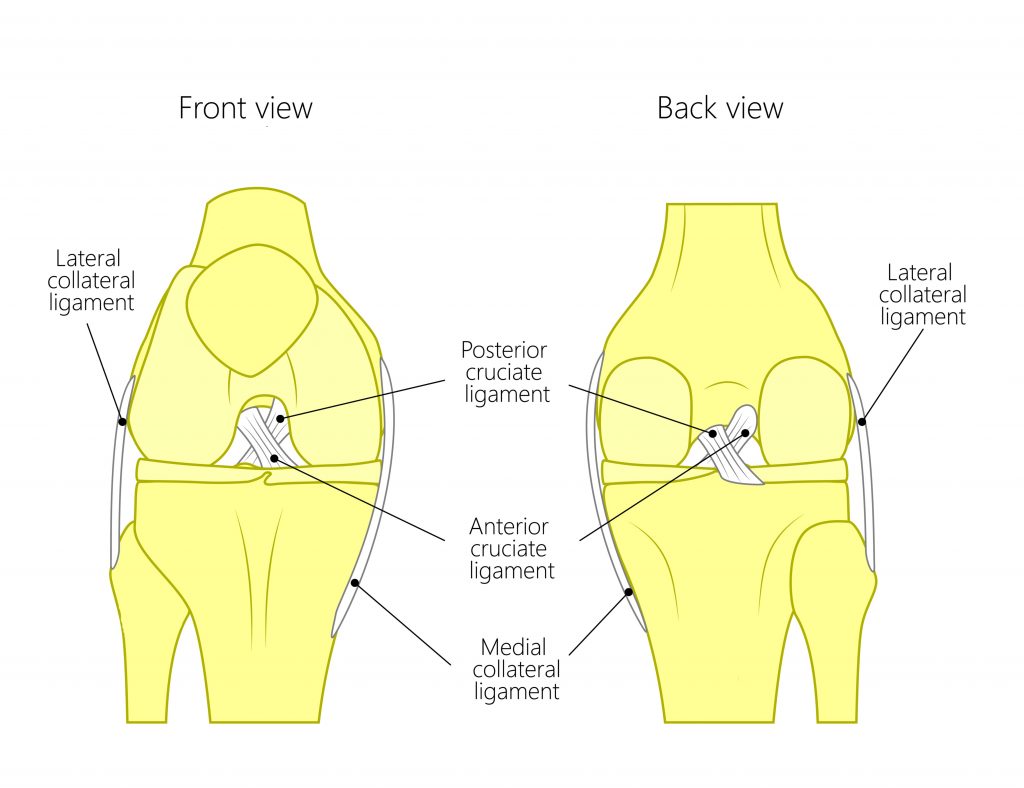
Connecting your bones together are the ligaments.
Covering the entire knee is a strong fibrous joint capsule. This contains a thick viscous fluid to help keep the knee lubricated.
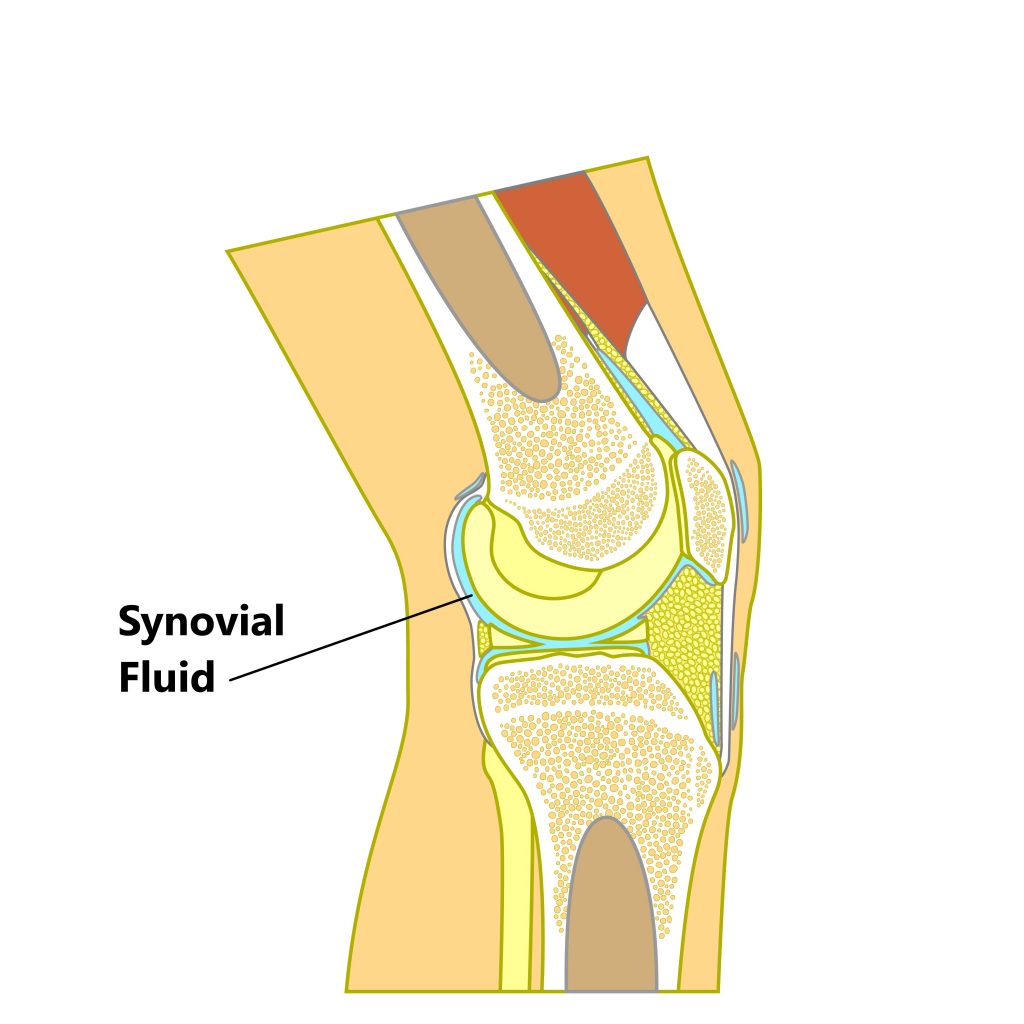
Small fluid filled sacs surrounding the knee called bursae to help reduce friction between the tendons, muscles and bones. The bursa at the back of the knee is continuous with the joint capsule.
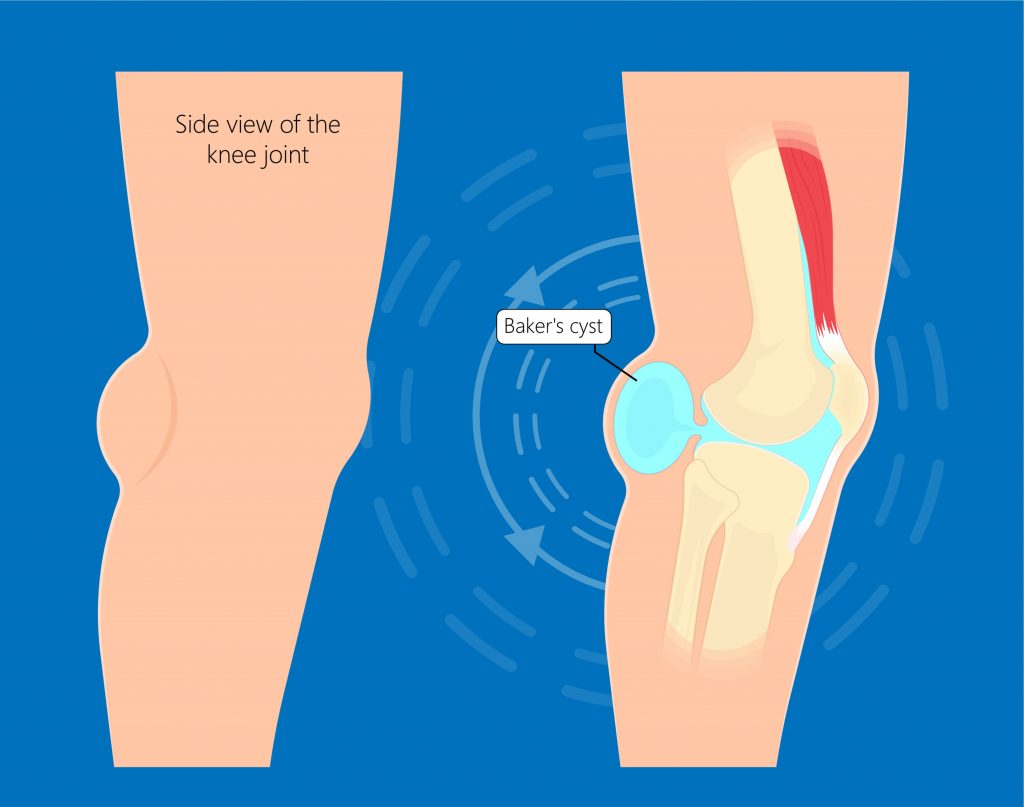
What is a Baker’s Cyst?
Excessive swelling and inflammation inside the joint capsule can cause the bursae at the back of the knee to swell and expand, this is known as a Baker’s cyst.
These do not normally cause any issues when they are small however, large Baker’s cysts can result in pain, limited movement, compression of nerves or compression of veins (increasing the chances of a blood clot forming in your veins).
What Causes a Baker’s Cyst?
Injury to any of the structures inside the joint capsule can cause excessive inflammation and swelling giving rise to a Baker’s cyst. Common causes include:
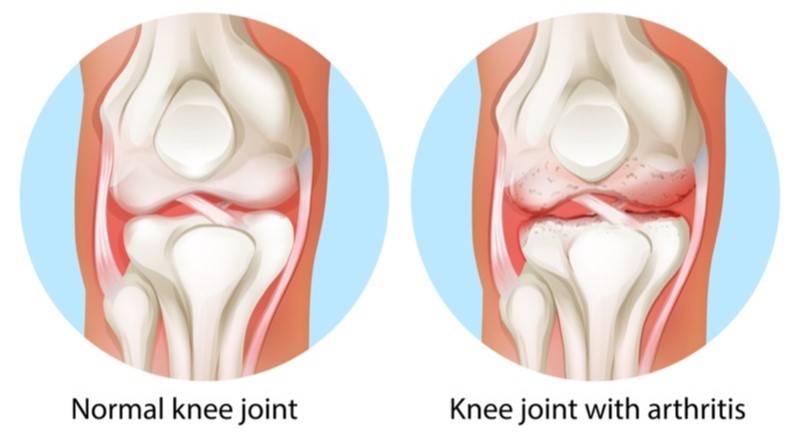
- arthritis
- meniscus injury
- ligament injury
- bone injury
- gout
Symptoms
- pain and stiffness at the back of the knee
- visible or palpable swelling at the back of the knee
- limited knee movement especially during bending
- increase in swelling and aggravation of symptoms with prolonged weight bearing activity
- pain into the calf (in cases where the cyst completely ruptures)

Diagnosis
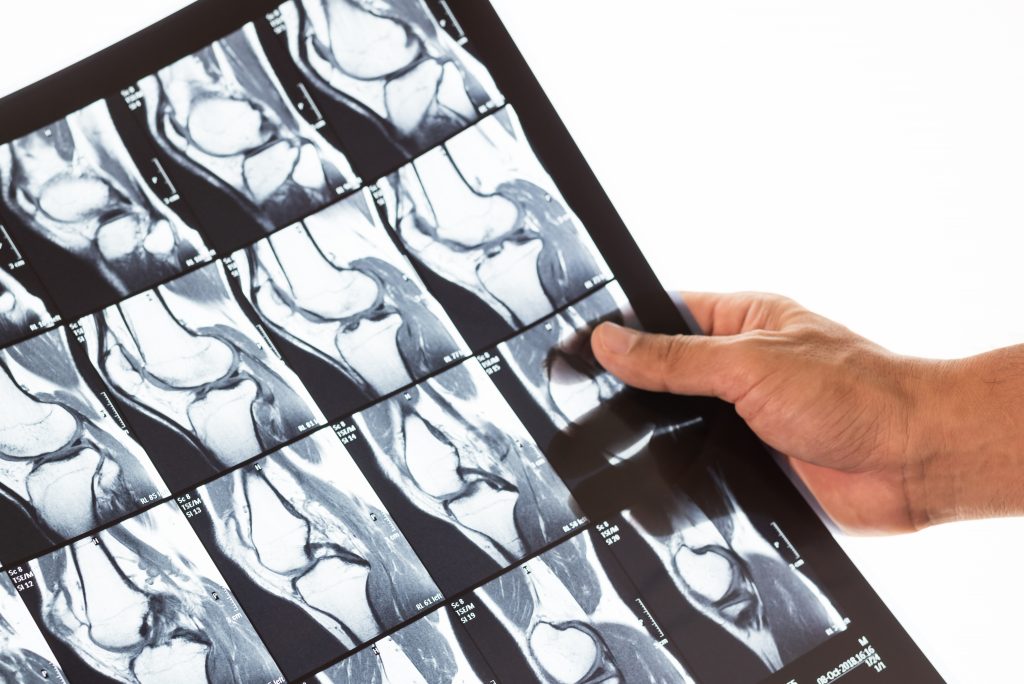
Diagnosing this condition is mainly based on an individual’s clinical presentation through a thorough subjective and physical examination. An X-Ray, ultrasound or MRI may also be required to assess the severity of the condition and to exclude/identify other injuries.
Management
Management should firstly be directed at the underlying cause of the inflammation (i.e. arthritis, meniscus injury). Drainage of a cyst will only provide short term temporary relief and are likely to reoccur. Small cysts often resolve with modified rest, conservative physiotherapy treatment (see below) and anti inflammatory medication. However, larger problematic cysts causing nerve/vein compression may require surgical excision.

Physiotherapy Management
- Reduce inflammation, swelling and decrease pain. Modalities such as RICE (Rest, Ice, Compression, Elevation), strapping, bracing and manual therapy may be used.

- Provide education regarding the injury, address unhelpful beliefs and identify and modify aggravating factors.

- Restore pain free knee range of motion and prevent secondary complications (i.e. secondary weight gain, calf shortening)

- Strengthen particularly the VMO muscle and other muscles surrounding the knee and hip joint.
- Regain balance and fine motor control.

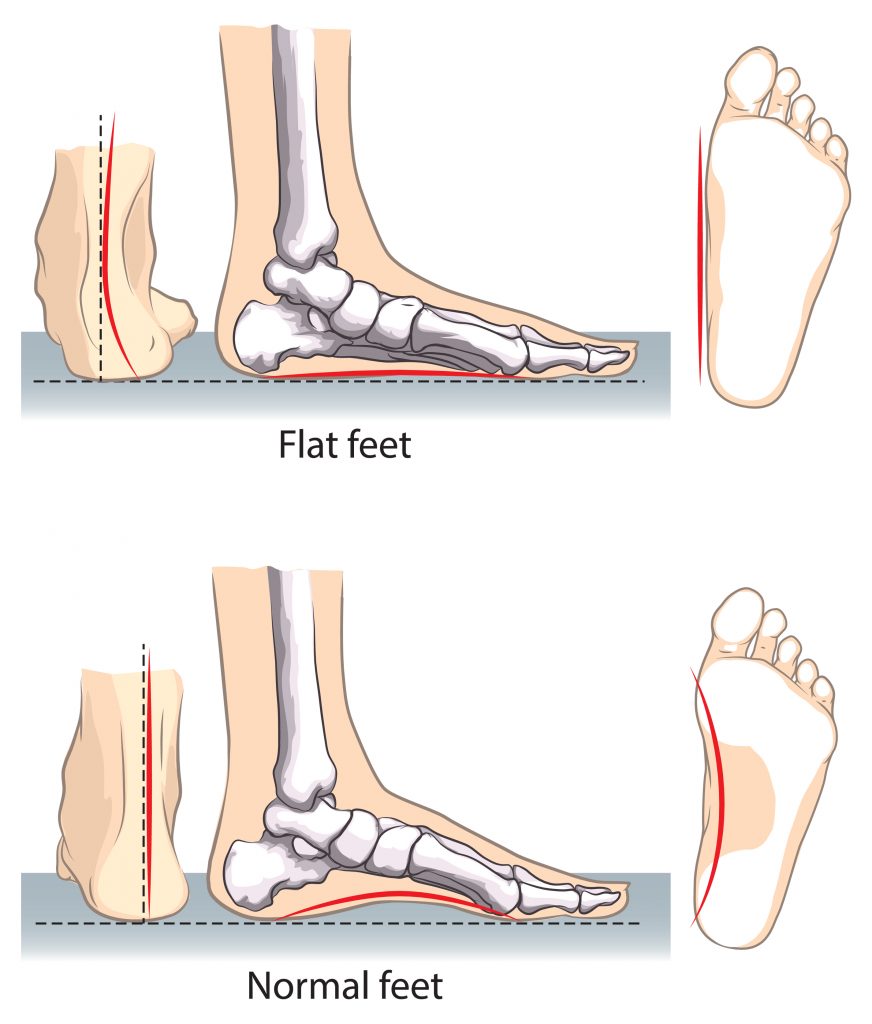
- Identify and address movement and postural issues that may have contributed to the injury (i.e. excessively flat feet, weak hip muscles).
Please keep in mind the information provided is general in nature and should not be used as a substitute to consult your treating health professional. If you have any specific questions or require assistance with your individual treatment requirements please do not hesitate to contact My Family Physio in Mona Vale, NSW.
Related Articles