Articles Stroke
This article explains what a stroke is, the different types of strokes, early warning signs, risk factors, acute management, recovery and rehabilitation.
Basic Anatomy
Your brain is much like a computer, it sends, receives and processes information throughout your entire body.
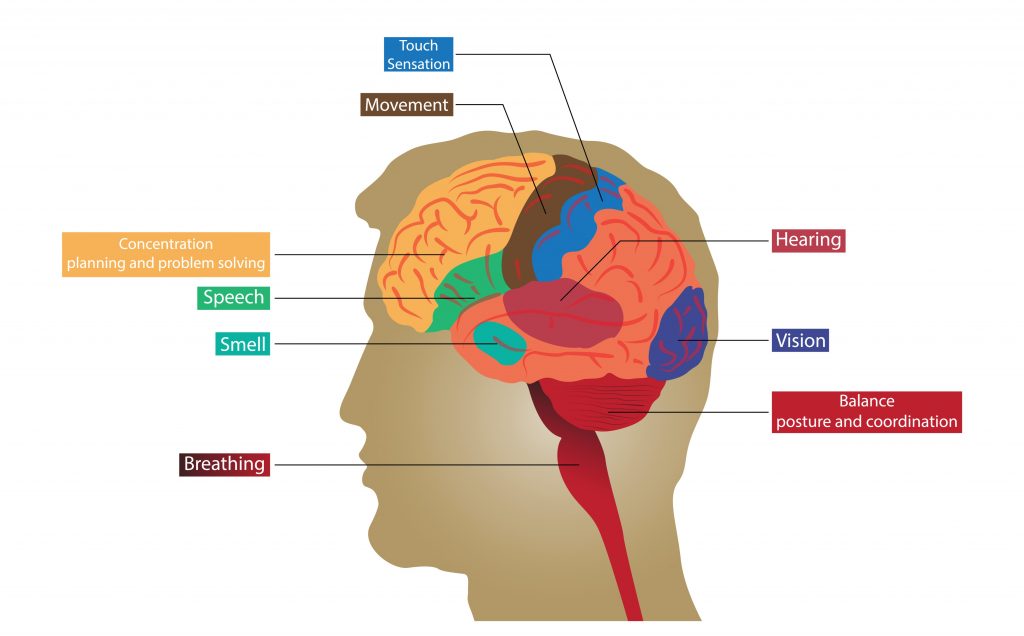
Each area of your brain is responsible for a different function (i.e movement, speech, emotions, problems solving, breathing, vision, hearing, balance, etc).
Pathways are formed between adjoining nerves to allow communication between each area. Much like a muscle, these pathways can be strengthened or weakened depending on how much they are used. This is why we get better at skills we practice more frequently (i.e. playing a musical instrument).

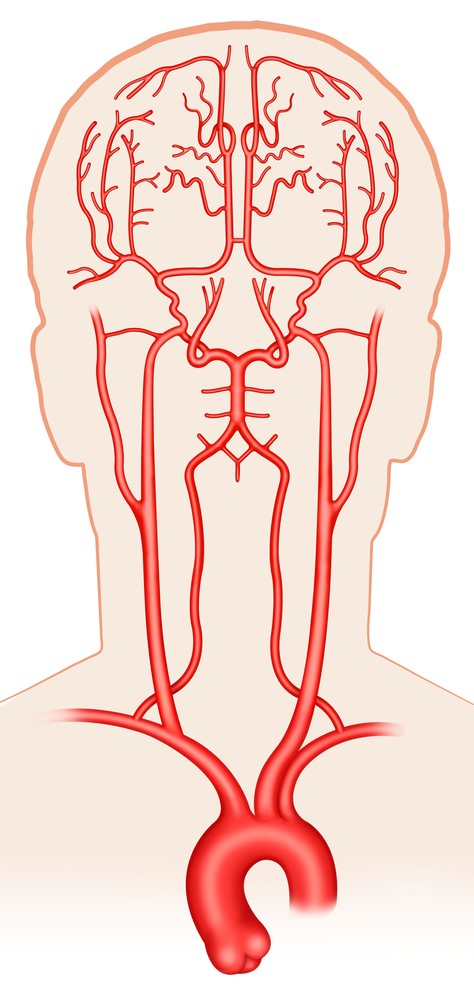
A network of arteries arising from your heart travel up through the neck to supply your brain with a constant supply of freshly oxygenated blood. Without this, your brain cells would begin to die. Unfortunately, brain tissue is very sensitive and this can start to happen within a matter of minutes.
What is a Stroke/Cerebrovascular Accident (CVA)?
Strokes affect approximately 1.7 % of the Australian population and are one of the leading causes of death and disability through out the world.
A stroke occurs when there is a disruption of blood flow to the brain. This can lead to cell death and irreversible damage. Depending on the location and size of a stroke, the symptoms and level of disability can vary greatly between individuals, in worst case scenarios a stroke can even lead to death.
What are the Different Types of Stoke?
TIA (Transient Ischeamic Attack)
A TIA is a mini stroke where there is a temporary blockage of blood flow to the brain. The symptoms will be similar to that of a stroke but will only last for a short period of time (minutes to hours). This is STILL a medical emergency and can be an early warning sign before having a full stroke.

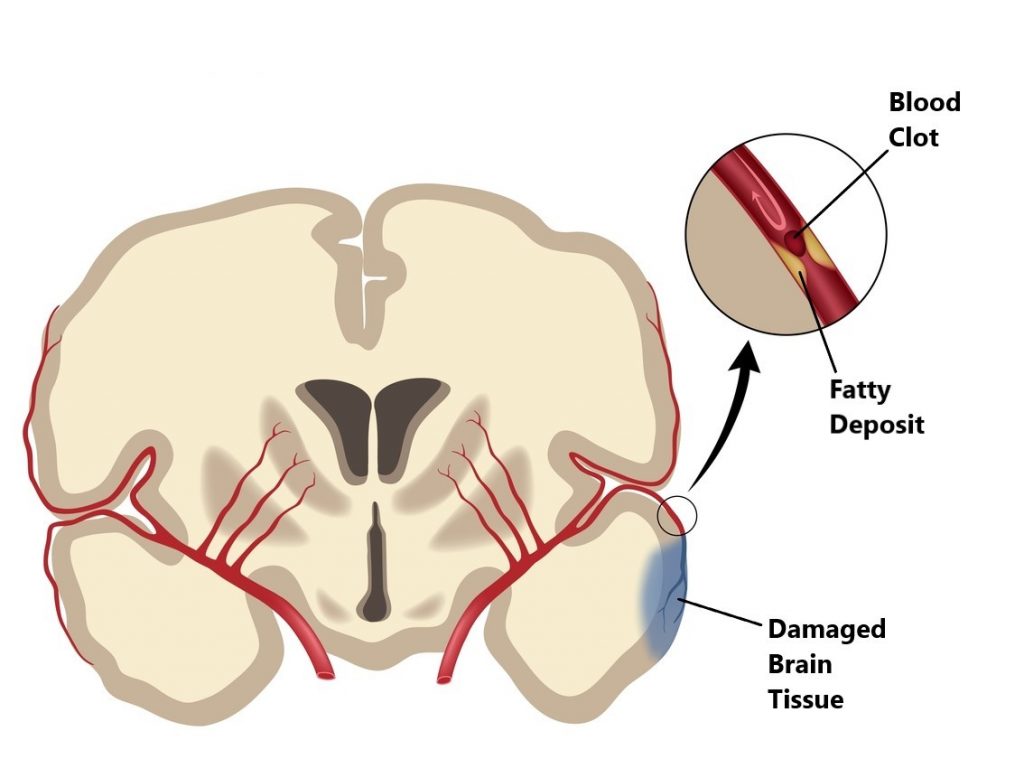
Ischaemic Stroke
These account for approximately 87% of all strokes and are due to a blockage of blood flow to the brain. Ischaemic strokes can be further categorised into 2 main types:
- Thrombotic stroke, caused by a blood clot forming in one of the blood vessels of the brain, these often occur in areas where there is a build up of fatty deposits causing narrowing of the artery.
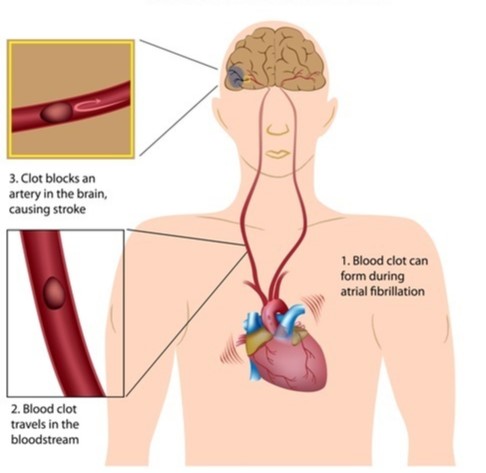
- Embolic stroke, caused by a blood clot forming in another area of the body (i.e. heart, lung) then travelling to one of the vessels of the brain.
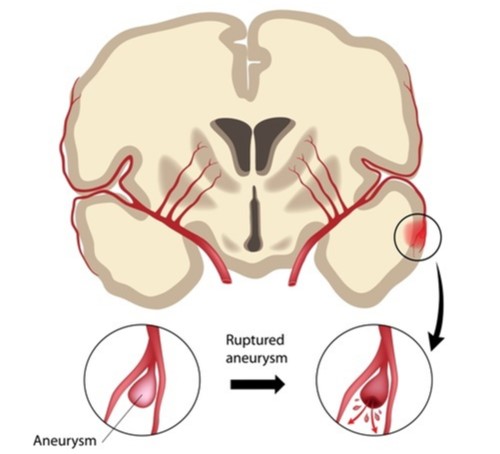
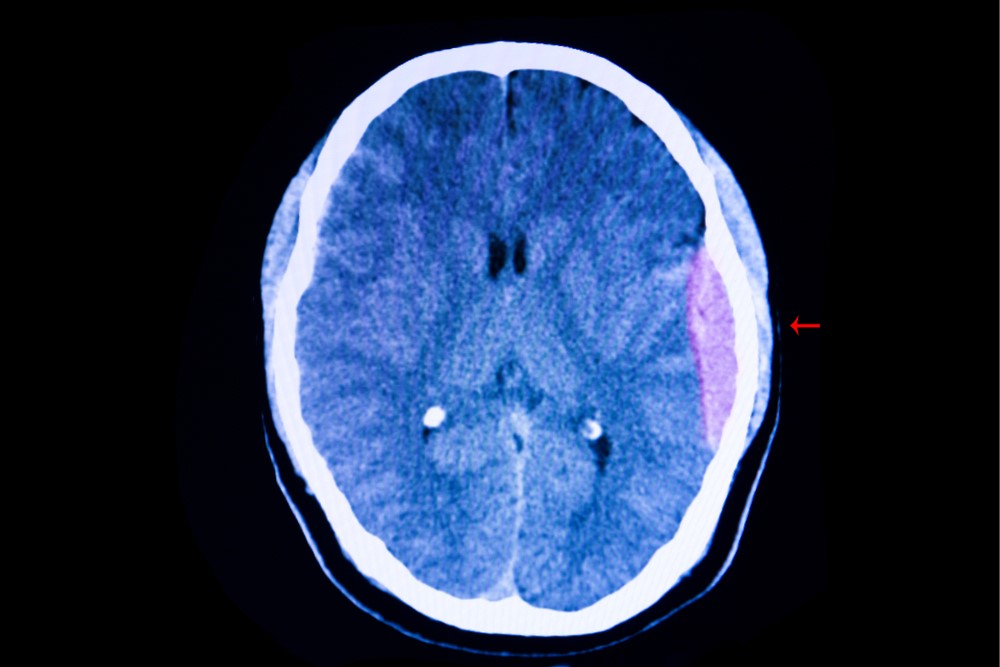
Hemorrhagic Stroke
These account for approximately 13% of all strokes and occur when a weakened blood vessel in the brain ruptures. This causes damage to the brain tissue due an accumulation of blood within the skull.
What are the Early Warning Signs of a Stroke?
- Sudden weakness or numbness in the face, arm, or leg on one side of the body.
- Sudden visual disturbances, particularly in one eye.
- Sudden difficulty speaking or trouble understanding speech.
- Sudden severe headache with no known cause.
- Sudden dizziness, loss of balance or sudden falls

Risk Factors
There are many risk factors associated with stroke. The good news is the risk of having a stroke can be reduced through lifestyle modification such as regular exercise, healthy eating, smoking cessation and limiting alcohol in take.
- high blood pressure
- history of smoking
- diabetes
- high blood cholesterol levels
- heavy drinking
- a diet high in fat (particularly saturated) and salt, but low in fibre, fruit and vegetables
- lack of regular exercise
- heart disease
- obesity
- history of TIA
- > 65 years of age
- family history
- female gender

What to do in the Event of a Stroke
A stroke is a medical emergency, it is always best to immediately call 000 and wait for an ambulance. Time is a critical factor in the acute setting as the amount of damage can be significantly lessened if treated quickly enough.
Acute Management
The aim of treatment in the acute setting is to medically stabilise the patient so that their condition does not deteriorate (i.e. maintaining blood pressure, breathing, circulation and vital organ function). In hospital the medical team will be able to quickly diagnose what type of stroke they are dealing with and identify what area of the brain has been affected, this will guide treatment.

Treatment of Ischemic Vs Hemorrhagic Strokes
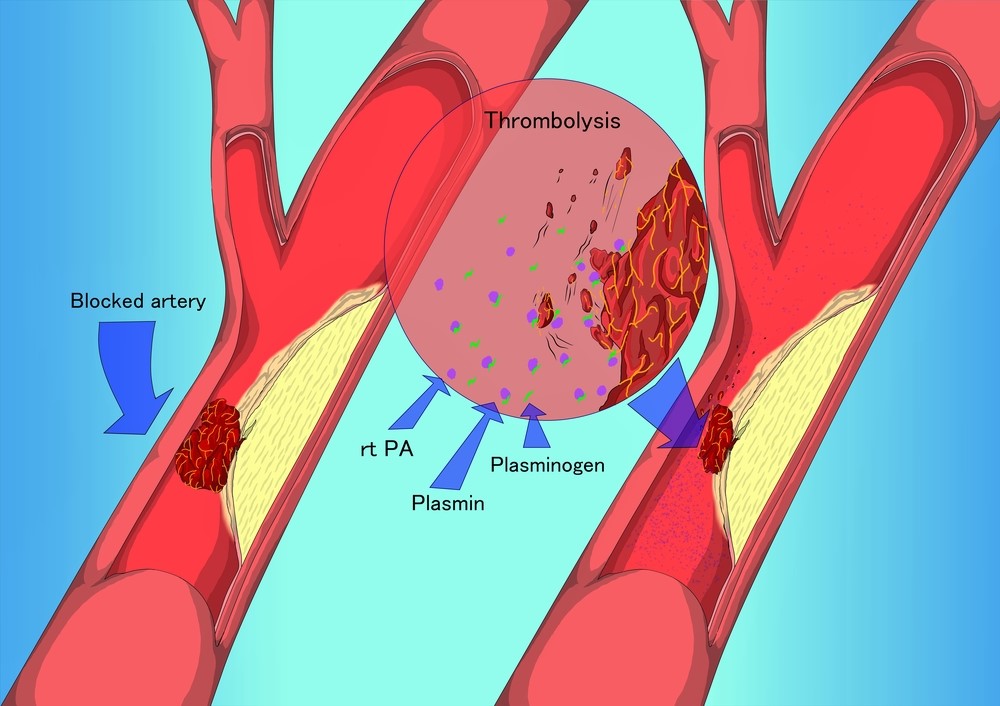
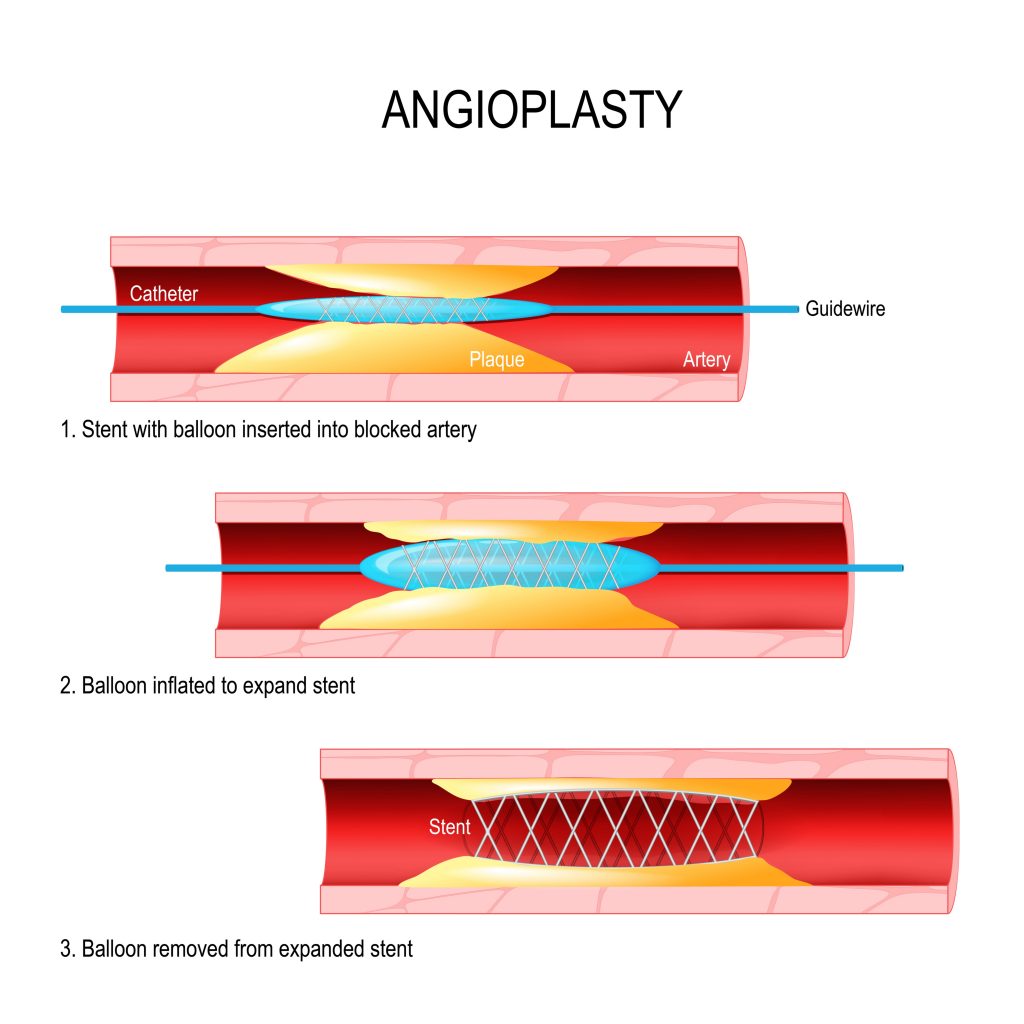
Treatment for ischemic strokes are aimed at restoring blood flow to the affected parts of the brain. This may involve:
- using medications and procedures to remove or dissolve blood clots
- surgery to unblock blood vessels
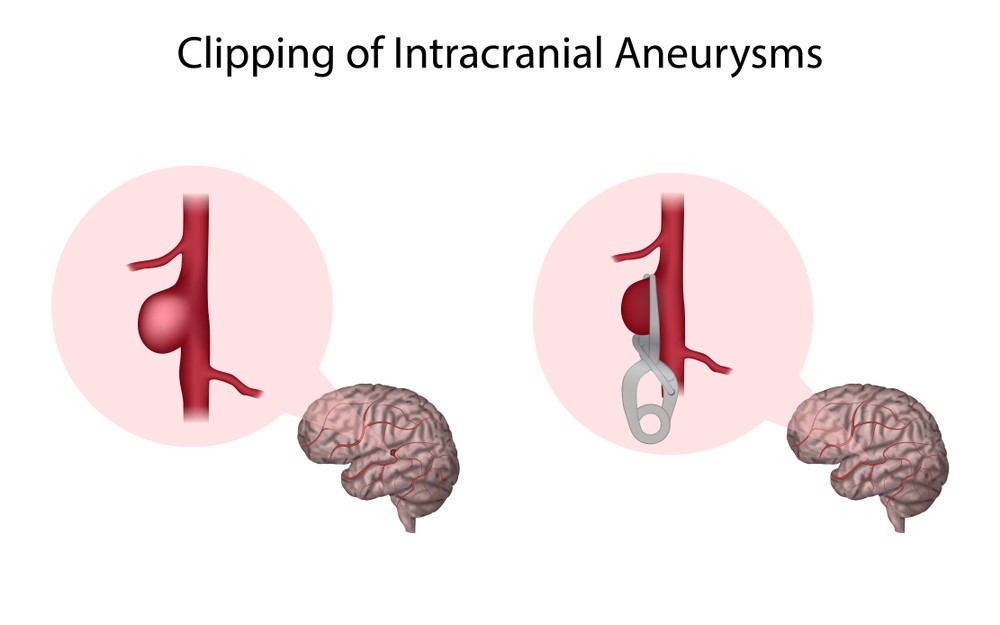
Treatment for hemorrhagic strokes are aimed at limiting the amount of bleeding and reducing the pressure placed on the brain. This may involve:
- ceasing blood thinning medications, using drugs to lower blood pressure and limit bleeding.

- Having a procedure or surgery to repair a ruptured blood vessel
- Having surgery to alleviate compression of the brain tissue.
Common Symptoms Following a Stroke
- sensation changes, numbness and chronic pain
- stiffening of muscles and joints (i.e. contractures, excessive muscle tone)
- loss of muscle tone and loosening of joints (i.e. subluxed shoulder)
- swelling in the arms and legs
- co-ordination and balance problems
- inability to use upper limb for functional tasks (i.e. feeding)
- muscle weakness (particularly down one side of the body)
- difficultly talking, swallowing and breathing
- reduced fitness
- restricted mobility
- decline in cognitive function
- incontinence
- depression
- trouble controlling emotions
- visual disturbances

Recovery Following A Stroke
Recovery following a stroke varies greatly between individuals. Some will make a near full recovery but the majority of people will be left with some kind of permanent impairment.

The severity of symptoms and level of disability is largely dependent on how large the stoke was and what areas of the brain have been affected. Most improvements will typically occur within the first 6 months however, some individuals can still make gains up to 2 years after the event.

Fortunately, our brains are fairly adaptable, connections between the nerves can be reestablished and new pathways formed in response to damage caused by a stroke. This process is best maximised through an intensive rehabilitation program. Like learning any new skill the key is repetition, persistence and practice.

The Rehabilitation Team
Rehabilitation following a stroke can commence as soon as an individual is medically stable and normally continues for at least 6 months after the event. The goal is to minimise disability and improve quality of life. Depending on an individual’s specific requirements, this may involve the assistance of several health professionals:
Doctors assist with:
- overseeing the rehabilitation process
- medically managing the patient so that rehabilitation can be optimised
- preventing secondary strokes and complications

Physiotherapists assist with:
- improving upper limb function
- regaining mobility
- improving cardiovascular endurance
- restoring function
- improving balance and coordination .
- improving swelling, joint, nerve and muscular pain

Speech Therapists assist with:
- regaining swallowing and speech functions
- assessing an individuals safety to consume certain foods/liquids
- improving memory, communication and cognition

Occupational Therapists assist with:
- regaining upper limb function
- improving cognition
- recommending aids, appliances and home modifications (i.e. rails, ramps, wheelchair) to facilitate function and promote independence.

Social Worker and Discharge Planners assist with:
- planning for new living arrangements if necessary (i.e. aged care facility)
- connecting an individual to financial resources (i.e. DVA, home care packages , NDIS)
- identifying community resources (i.e. community nursing)

Please keep in mind the information provided is general in nature and should not be used as a substitute to consult your treating health professional. If you have any specific questions or require assistance with your individual treatment requirements please do not hesitate to contact MyFamily Physio in Pittwater Place Shopping Centre in Mona Vale.
Related Links