Articles ITB (Iliotibial Band) Syndrome
This article covers basic anatomy, what ITB syndrome is, symptoms, causes, risk factors, diagnosis, medical and physiotherapy management.
Basic Anatomy
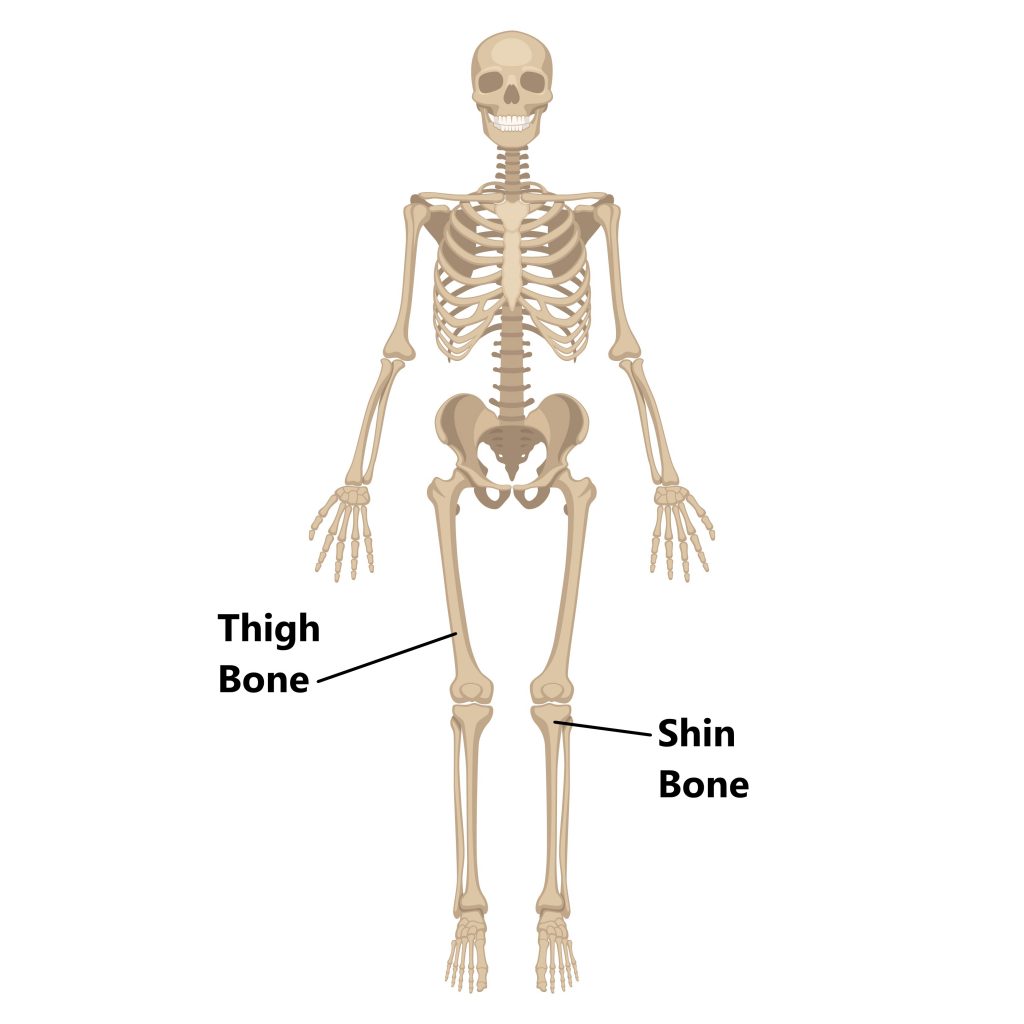
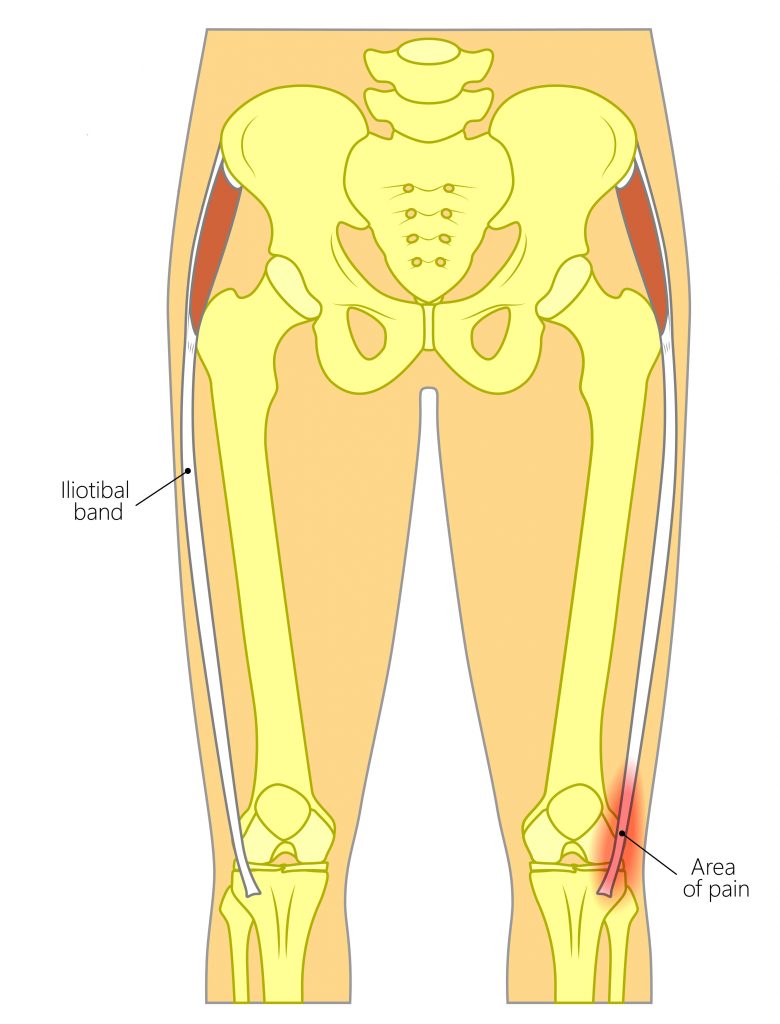
The bones of your thigh and shin form the main joint of your knee.
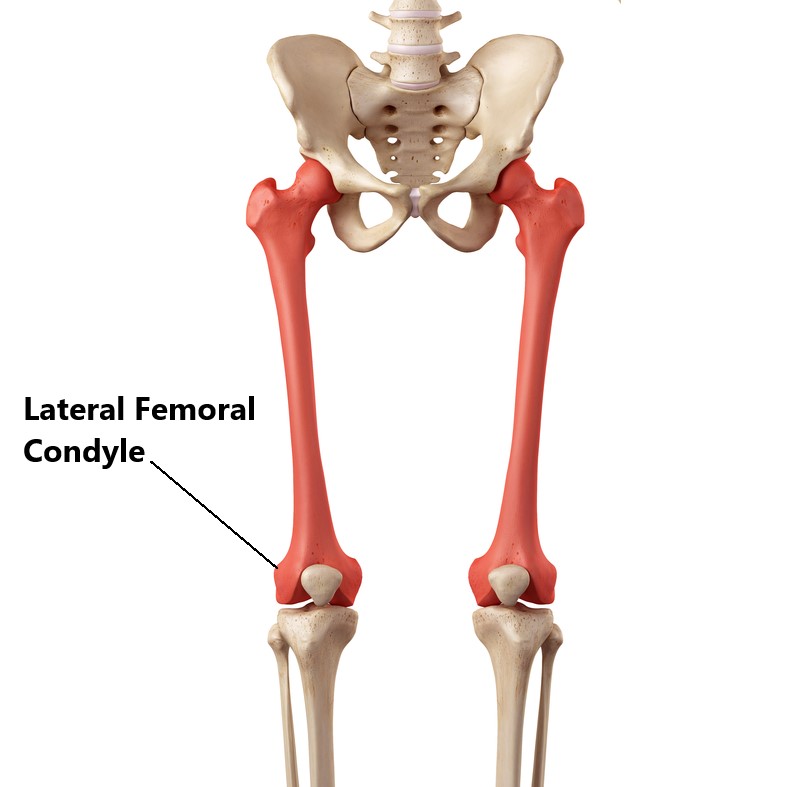
Towards the lower end of your thigh, the bone starts to flare out forming a bump on either side. These bumps are the attachment sites for several tendons, muscles and ligaments. The bump on the outside is known as the lateral femoral condyle.
What is the Iliotibial band (ITB) ?
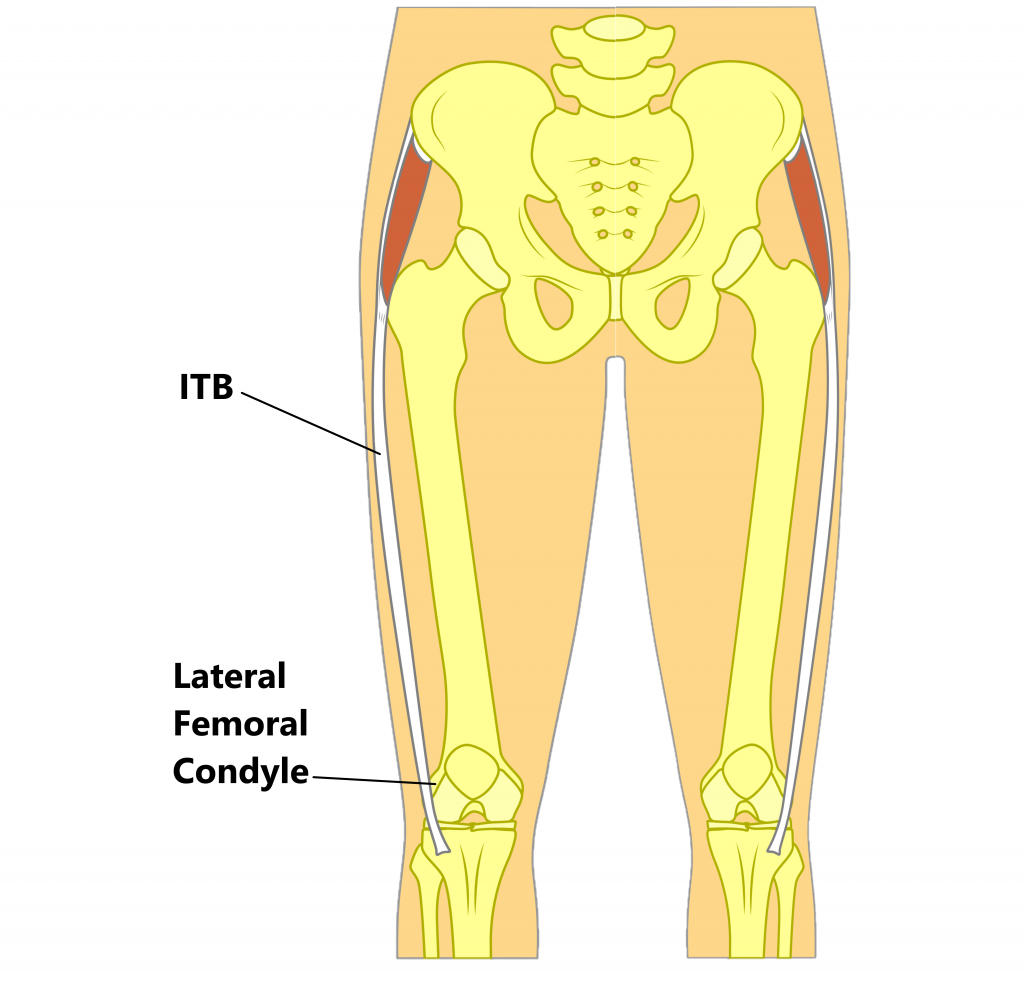
Running along the entire outside length of your thigh is a band of tough fibrous tissue called the ITB. It originates from several muscles in your hip and inserts just below the knee.
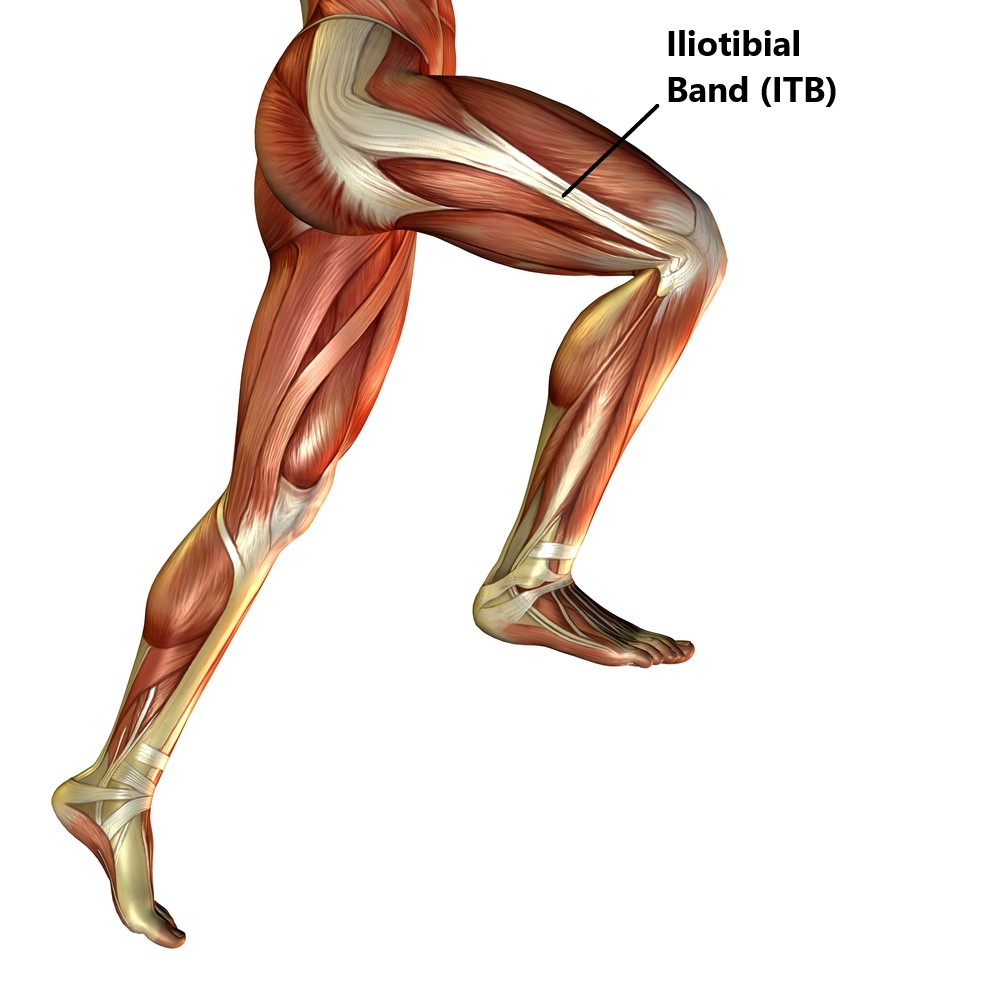
This structure also overlies the lateral femoral condyle.
What is ITB Syndrome?
As your knee is bent and straightened your ITB flicks over the lateral femoral condyle. This repeated action can eventually give rise to excessive friction causing inflammation and pain on the outer side of your knee, this is known as ITB syndrome. This is typically an overuse condition and most commonly seen in distance runners and cyclists due to the repetitive nature of their sports.
What are the Symptoms of ITB Syndrome?
- pain or burning on the outside of the knee
- swelling on the outside of the knee
- aggravation of symptoms with downhill running or descending stairs
- worsening of symptoms as activity continues
- pain during the running/walking motion particularly as the heel first hits the ground and the knee starts to bend

What are the causes of ITB syndrome?
ITB syndrome is often due to a combination of several factor this commonly includes:
Excessive Activity, sudden increases in activity (i.e. increasing distance, commencing a new fitness regime, introducing weights) do not give your body enough time to adapt to the additional loads placed upon it. Failure to modify activity will result in prolonged symptoms. This is often a major contributing factor in the majority of individuals presenting with ITB syndrome.

Training surfaces, training on sloping (i.e. down hills/stairs) or uneven (i.e. sand) surfaces place more strain on your ITB as your knee straightens and bends.

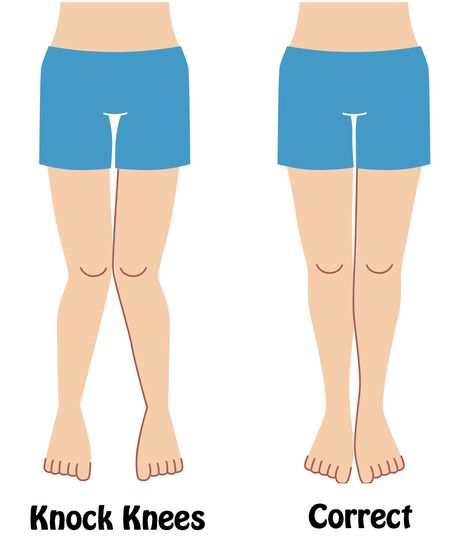
Excessive “Rolling In” of the Knees, this abnormal position places more tension on the ITB as it flicks over the lateral femoral condyle. This is often due to:
- weak gluteal and core muscles
- excessively tight leg muscles
- flat feet
- inadequate foot wear
Diagnosis
Diagnosing this condition is mainly based on an individual’s clinical presentation through a thorough subjective and physical examination. An xray, ultrasound or MRI may also be required to exclude/identify other injuries.

The lateral femoral condyle is compressed as the knee is straightened from a 90 degree position. A positive test will reproduce symptoms as the knee is nearly in a straightened position.
Risk Factors
- participating in distance running, cycling or endurance sports
- uneven leg length
- excessive knock kneed or bow legged posture
- flat feet

Treatment
- anti inflammatory medications (i.e. Voltaren, Neurophen)
- physiotherapy treatment (see below)
- cortisone injection to reduce inflammation
- surgery is rare and only indicated in severe long standing cases where conservative treatment has failed.

Physiotherapy Management
- Reduce inflammation and decrease pain. Modalities such as RICE (Rest, Ice, Compression, Elevation), taping and manual therapy may be used

2. Provide education, identify and modify aggravating factors (i.e. changes to training regime)

3. Restore pain free hip and knee range of motion

4. Strengthening of the hip and core muscles

5. Correction of posture (i.e. foot and knee posture, leg length discrepancies)

6. Identify and address movement and postural issues that may have contributed to the injury (i.e. running technique, cycle set up)

Please keep in mind the information provided is general in nature and should not be used as a substitute to consult your treating health professional. If you have any specific questions or require assistance with your individual treatment requirements please do not hesitate to contact My Family Physio in Mona Vale.
Related Articles