Articles Ankylosing Spondylitis
This article explains what ankylosing spondylitis is, causes, affected areas, progression, symptoms, risk factors, diagnosis and management.
What is Ankylosing Spondylitis (AS)?
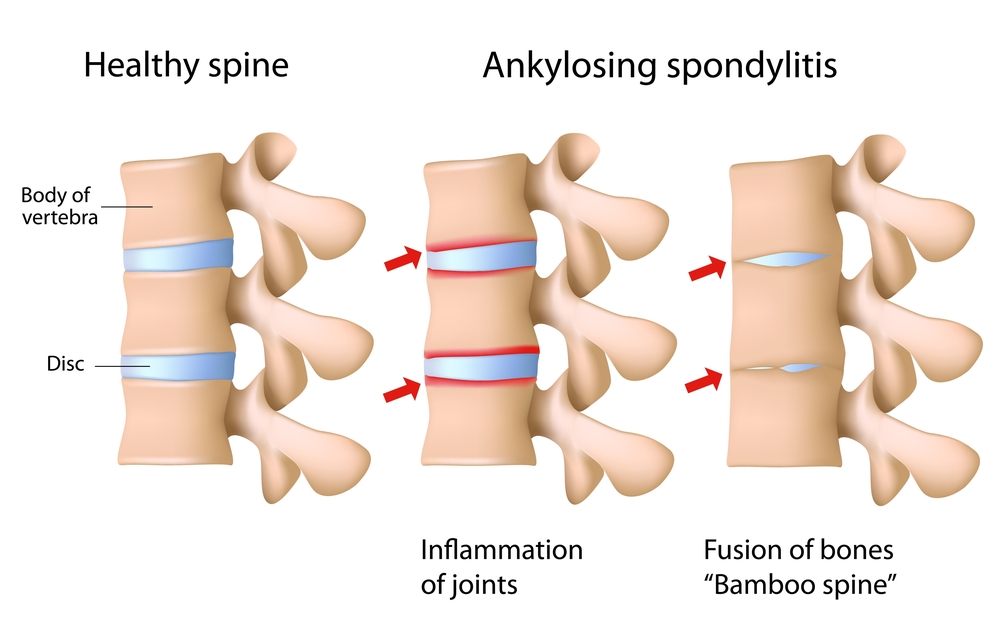
AS is a type of inflammatory arthritis which mainly affects the joints of the spine and pelvis. It can lead to ongoing pain and stiffness. This is an autoimmune condition, meaning your bodies defence system mistakenly starts to attack its own tissues.

What Causes Ankylosing Spondylitis ?
AS affects approximately 0.1 – 0.2% of the population. Unfortunately, researchers have not yet been able to identify the underlying cause of this disease. There appears to be a strong genetic component as 95% of individuals with AS carry the HLA-B27 gene. (Please Note: this gene is also fairly common within the general population, only 1 in 8 people with this gene will actually develop AS).
What Areas of the Body Does Ankylosing Spondylitis Affect?
- Spinal joints of the neck, upper and lower back
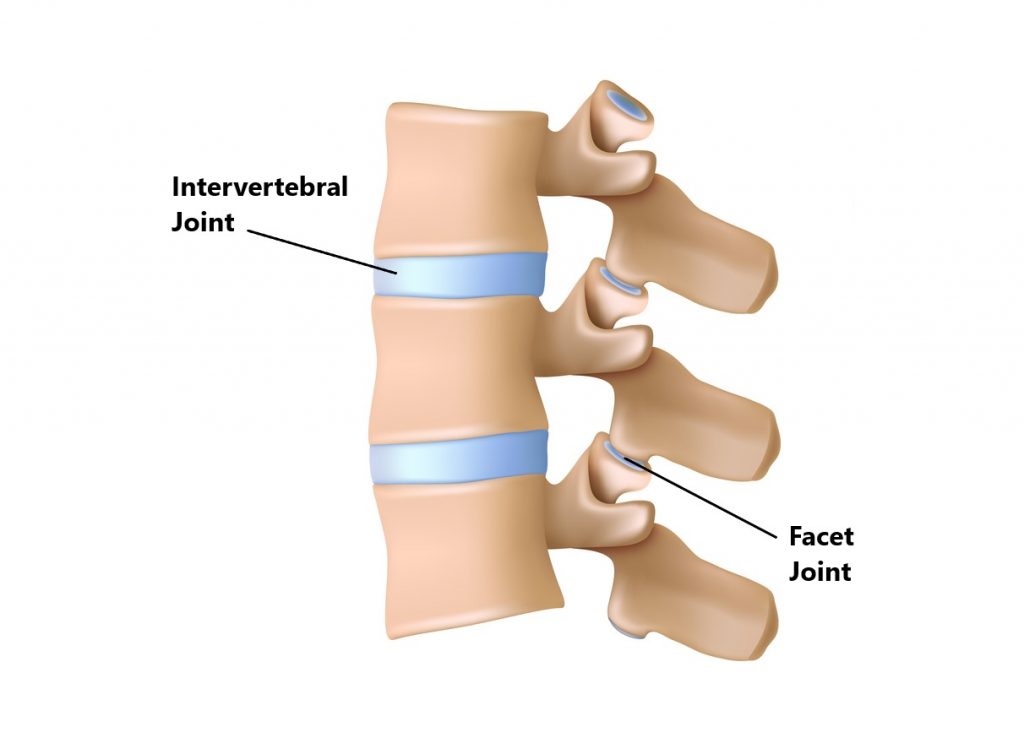
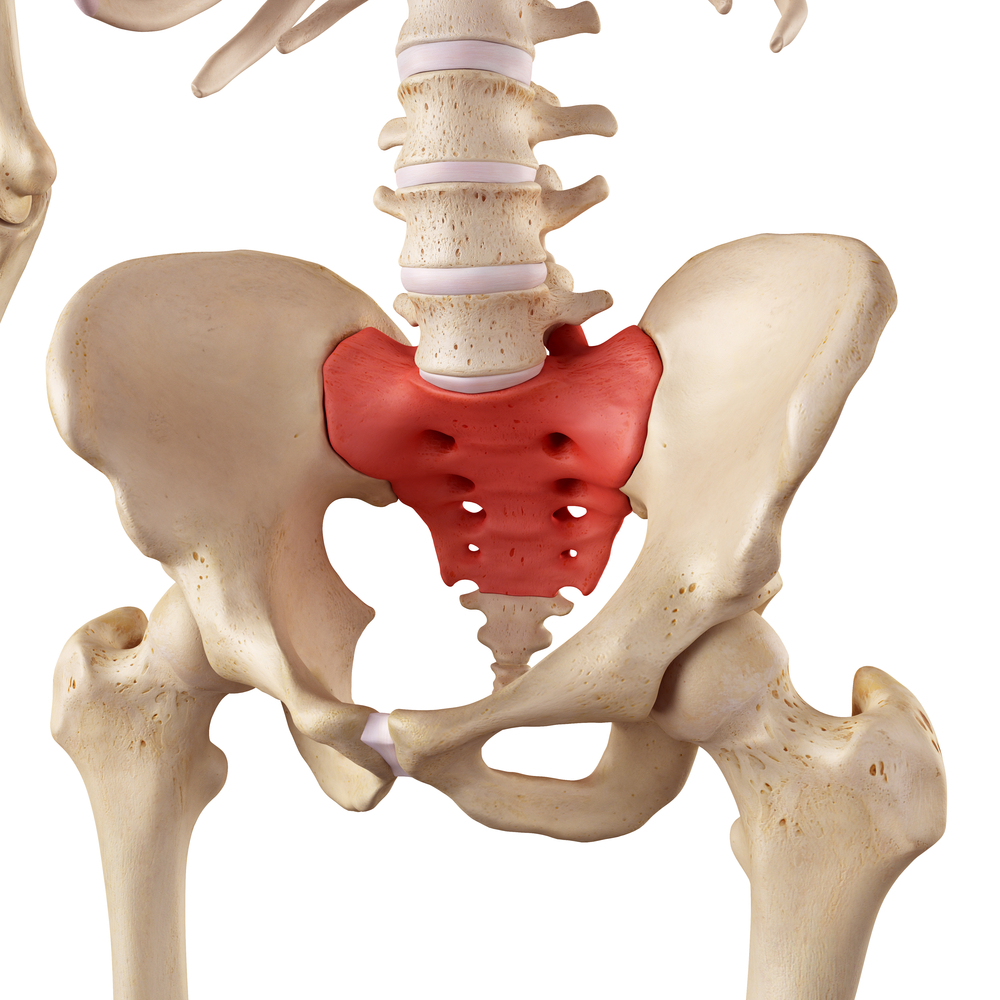
- Joints of the sacrum/buttock area
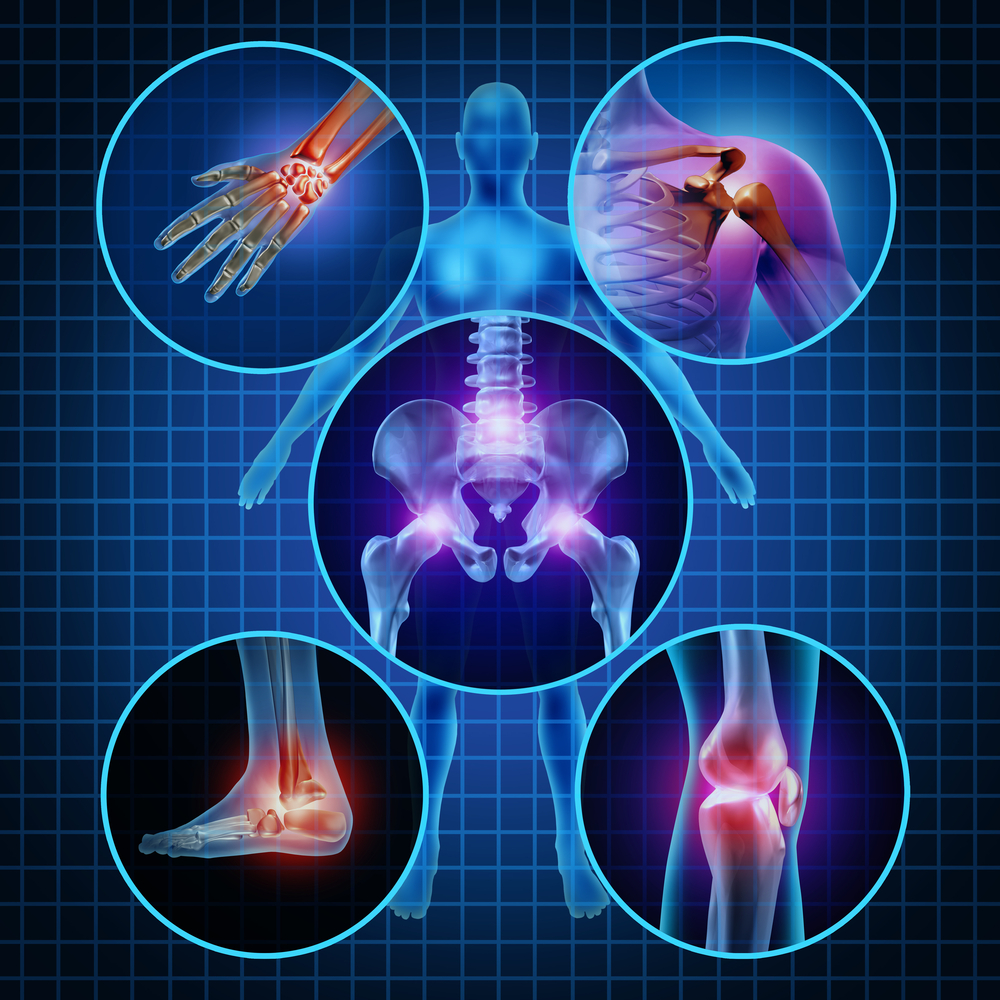
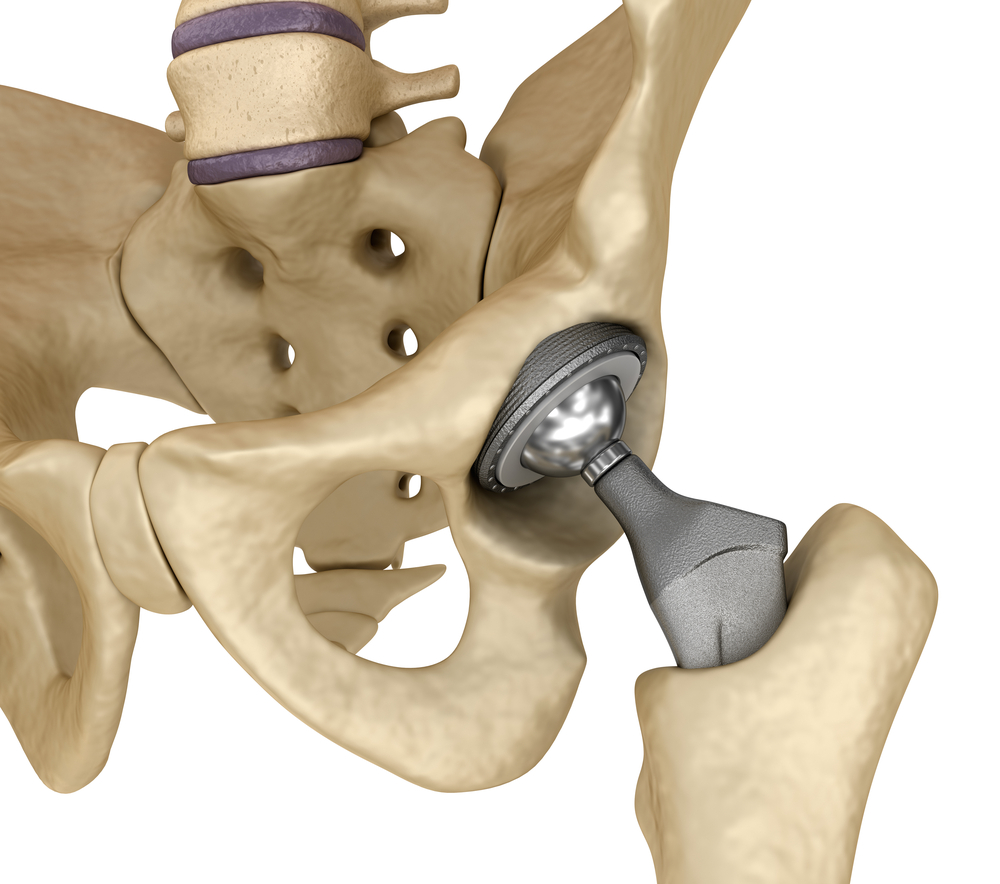
- The major joints of the body (i.e. hips, knees, shoulder and ankles)
- Joints of the rib cage
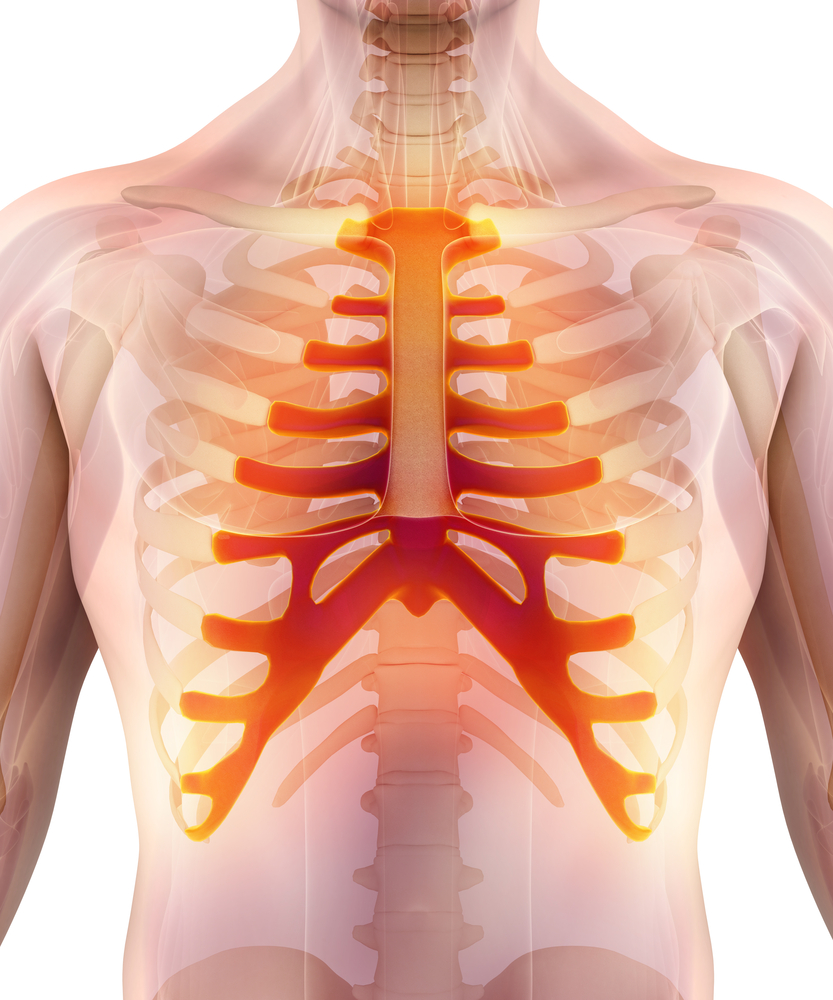
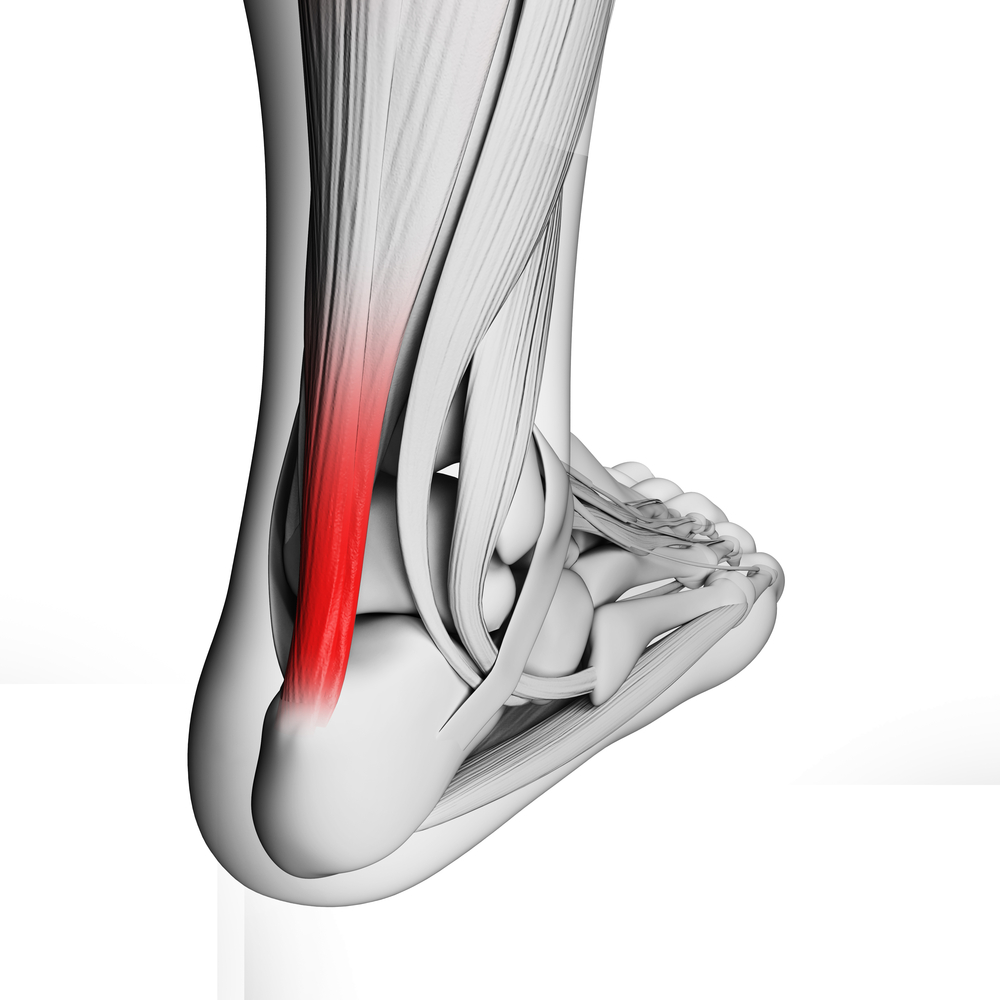
- Where tendons and ligaments attach on to the bone (heels, knees, ankles)
- Can also result in inflammation of the eye, skin, lung and bowel tissue

Does Ankylosing Spondylitis Progress Over Time?
Unfortunately, AS can progress over time. Affected individuals often have episodes where their symptoms flare up followed by a period of remission. Over time this repeated cycle can cause excessive bone formation and eventually lead your joints fusing together. This can drastically impact an individuals movement, level of function and quality of life.
Symptoms
The first signs of AS commonly arise between the ages of 15-45 years. Unlike other types of musculo skeletal pain, the symptoms of AS gradually occur over a period of time without an aggravating event (i.e. fall, lifting injury). Symptoms will generally persist for at least 3 months.
- stiffness in the morning
- symptoms improved with heat (i.e. hot shower)
- restricted movement
- bilateral symptoms (i.e. both sides of your buttock)
- stooped posture
- symptoms relieved with exercise and worse after rest
- constant buttock an spinal pain
- swollen joints
- disturbed vision
- upset bowel
- problems with breathing and fitness
- skin rash
- fatigue

Risk Factors
- Having a family history of AS
- More common in males than females (3:1)
- More often observed in Caucasians
Diagnosis
Diagnosis of AS is based on a thorough subjective and objective clinical examination. Normally, your GP will order blood tests (for inflammatory markers and presence of the HLA- B27 gene) and imaging (xray, CT, MRI) to confirm the diagnosis. Most confirmed cases are often referred to a Rheumatologist for management.

Abnormal findings on imaging will only be detected in the later stages of the disease
Management
Unfortunately there is no cure for AS. However, appropriate treatment can help to alleviate symptoms and slow down the progression of the disease. This can include:
- Physiotherapy treatment (see below)
- Medications for pain relief
- Medications to reduce inflammation
- Medications to dampen your immune response
- Surgery may be required in rare circumstances as a result of excessive bone formation (i.e. joint replacement, decompression of spinal nerve tissue)
Physiotherapy Management
- Reduce inflammation and decrease pain. Modalities such as modified rest, strapping, manual therapy and acupuncture may be used.
- Provide education regarding the injury, address unhelpful beliefs, identify and modify aggravating factors
- Restore pain free range of motion and return to basic activities. Commence gentle stretches, hydrotherapy or a walking program
- Restore strength of the core and lower limbs. Commence a graded strengthening program.
- Improve nerve flexibility. Commence specific nerve stretching exercises.

Gluteal Stretch



Please keep in mind the information provided is general in nature and should not be used as a substitute to consult your treating health professional. If you have any specific questions or require assistance with your individual treatment requirements please do not hesitate to contact My Family Physio in Mona Vale, Northern Beaches of Sydney.
Related Articles