Articles Polymyalgia Rheumatica
This article explains what Polymyalgia Rheumatica is, causes, symptoms, risk factors, diagnosis, medical and physiotherapy management.
What is Polymyalgia Rheumatica (PMR)?
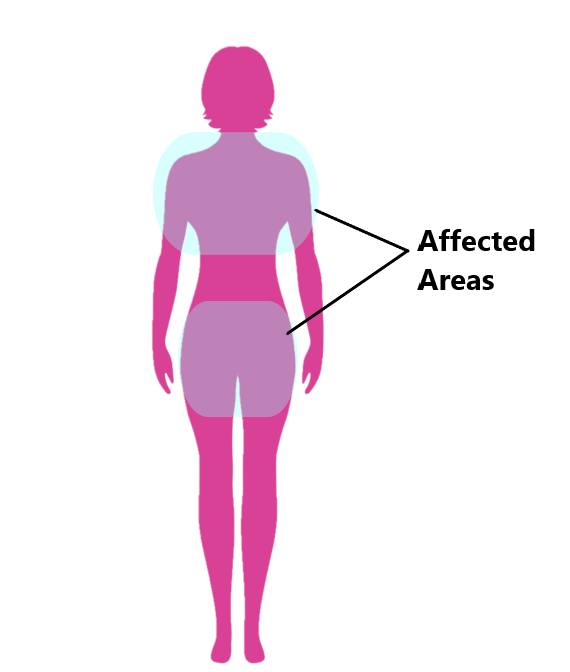
PMR is a type of inflammatory disorder which gives rise to widespread pain and stiffness in the neck, shoulders, arms and/or hips. It typically affects older individuals and is rarely seen in people below the ages of 50 years.
It can cause inflammation and swelling of the joints, muscles and surrounding soft tissues (i.e. bursa). Thankfully, PMR does not cause permanent joint damage. However, it can significantly impact an individual’s quality of life by making simple everyday tasks difficult and to perform such as getting dressed, washing their hair or getting up out of a chair.
What Causes Polymyalgia Rheumatica?
Unfortunately, the causes of this disease are not very well understood. Many researchers believe PMR is an autoimmune condition, meaning your body’s defence system mistakenly starts to attack its own tissues giving rise to pain and inflammation.
What are the Symptoms of Polymyalgia Rheumatica?
The symptoms of PMR typically develop over a short period of time (days/weeks) and often come on spontaneously without a cause. This can include:
- muscle pain and stiffness, especially in the neck, shoulders, arms and hips
- increased symptoms in the morning or following a prolonged period of rest (i.e. sitting down to have lunch)
- alleviation of symptoms throughout the day only to return in the evening
- restricted movement in the neck, shoulder arms or hips (i.e. inability to lift your arm above your head)
- symptoms often affect both left and right hand sides of the body

These symptoms may also be accompanied by the signs of chronic inflammation:
- mild fever
- fatigue
- generally feeling unwell
- loss of appetite
- weight loss
- depression
PLEASE NOTE: It is very important to seek urgent medical attention if you experience headaches or visual disturbances in addition to the other symptoms associated with PMR. This can be a sign of a more serious condition called giant cell arteritis which can be related to PMR.

What are the Risk factors of Polymyalgia Rheumatica?
Risk factors for PMR include:
- The highest incidence of PMR is seen in individuals >70 years of age
- Females are 3 times more likely to develop PMR than males
- PMR is most often observed in people who are of Caucasian descent
- Family history of PMR

How is Polymyalgia Rheumatica Diagnosed?
Diagnosing PMR can be difficult, many other medical conditions can give rise to similar symptoms and will need to be excluded (i.e . rheumatoid arthritis). There is no single test for PMR , your doctor will make their diagnosis based on a:
- subjective examination (i.e. marked stiffness in the morning, fatigue, symptoms lasting for >2wks)
- physical examination (i.e. bilateral symptoms, restricted movement, patient age)
- blood tests (to check inflammatory markers)
- scans (to exclude musculoskeletal causes)

Medical Management
Unfortunately, there is no cure for PMR and the treatments available are to help alleviate symptoms.
This condition is typically managed with corticosteroids (i.e. prednisone), these medications are powerful antiinflammatories and can only be prescribed by your doctor. Corticosteroids should not be confused with non steroidal antiinflammatories (i.e. voltaren, nurofen), these too have antiinflammatory properties however they are less effective and do not require a doctor’s prescription.
It is common for individuals with PMR to have episodes where their symptoms “flare up” followed by a period of remission. These episodes can last from several months to several years. Your medications will be adjusted depending on the severity of your symptoms. Long term use of corticosteroids can be harmful (i.e. osteoporosis, high blood pressure, diabetes) therefore, these medications will need to be weaned down over time.

Physiotherapy Management
- Reduce pain and stiffness. Modalities such as modified rest, strapping, manual therapy and acupuncture may be used.
- Provide education regarding the injury, identify and modify aggravating activities

- Restore pain free range of motion

- Restore strength

Please keep in mind the information provided is general in nature and should not be used as a substitute to consult your treating health professional. If you have any specific questions or require assistance with your individual treatment requirements please do not hesitate to contact My Family Physio in Mona Vale.