Articles Intervertebral Disc Injuries
This article outlines simple anatomy, common injuries and management principles to give the you a good basic understanding of intervertebral disc injuries.
Basic Anatomy
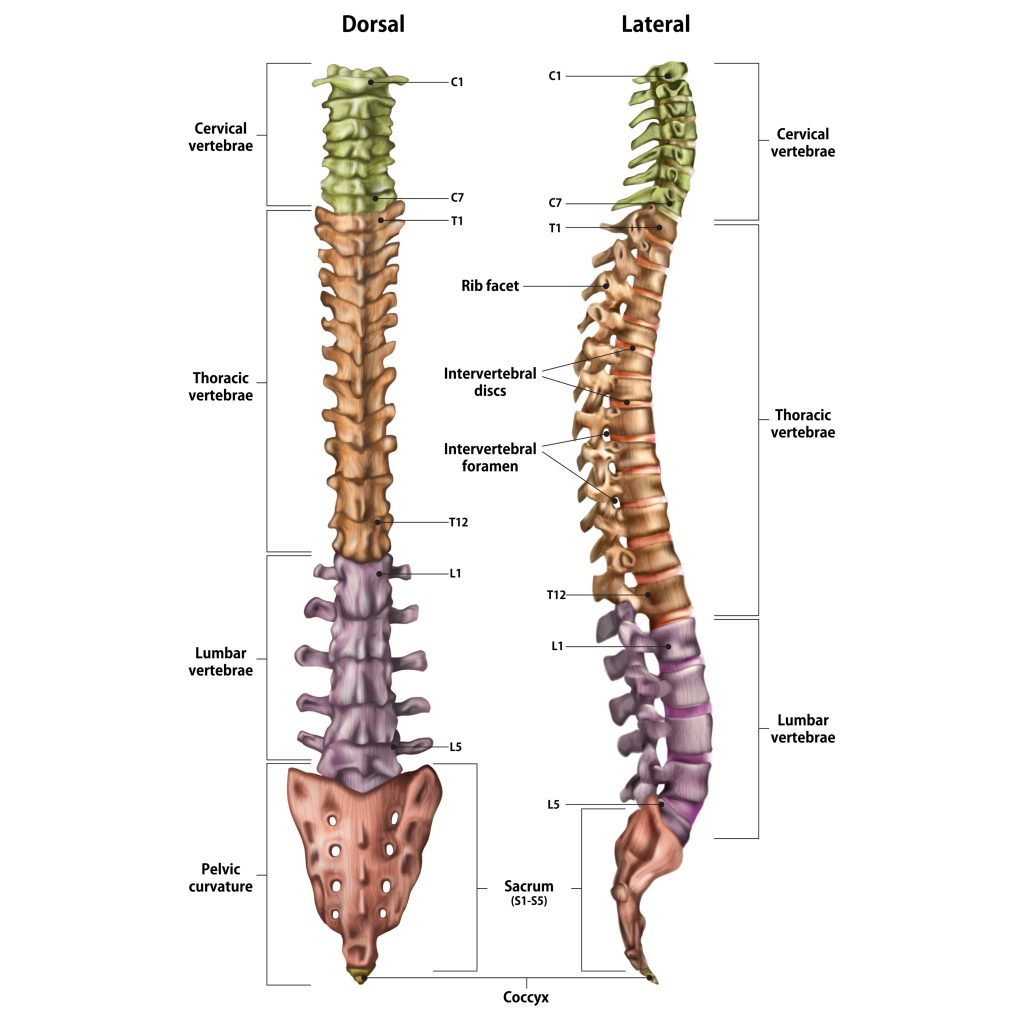
The spinal column is made up of individual bones called vertebrae and named accordingly to their position in the spine (see below). The spine is divided into 4 sections:
- Cervical spine (neck) C1-C7
- Thoracic spine (upper back) T1-12
- Lumbar spine (lower back) L1-5
- Sacrum (pelvic area) S1
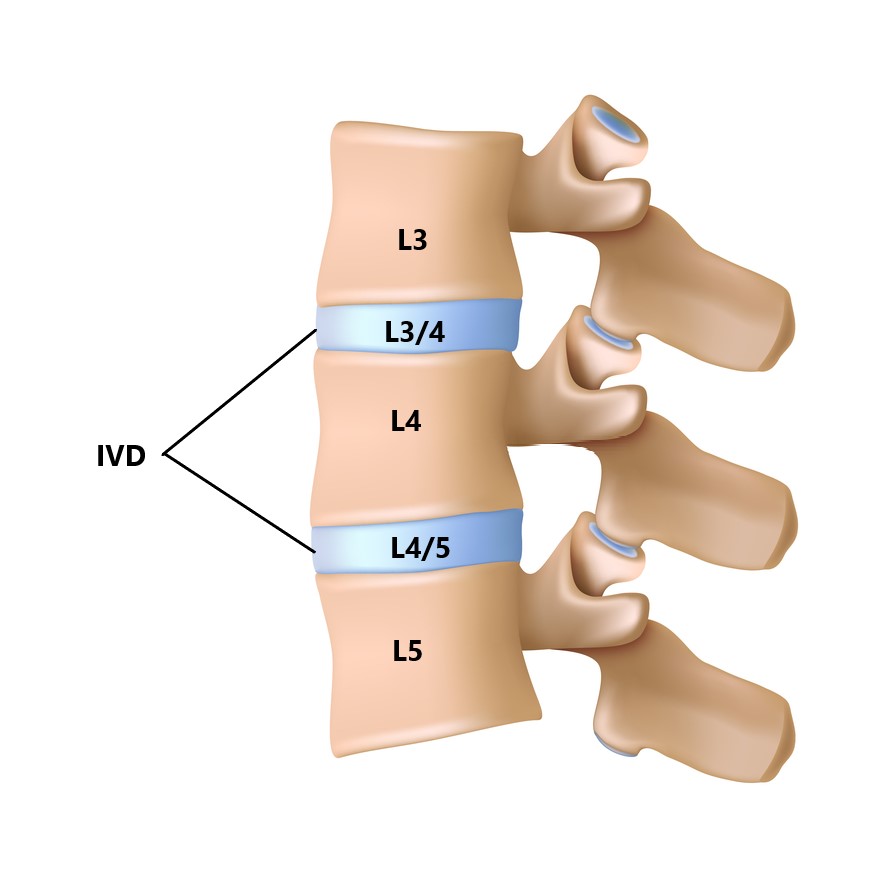
Between each vertebrae is an intervertebral disc (IVD). Each IVD is named relative to the vertebrae they sit between (see below)
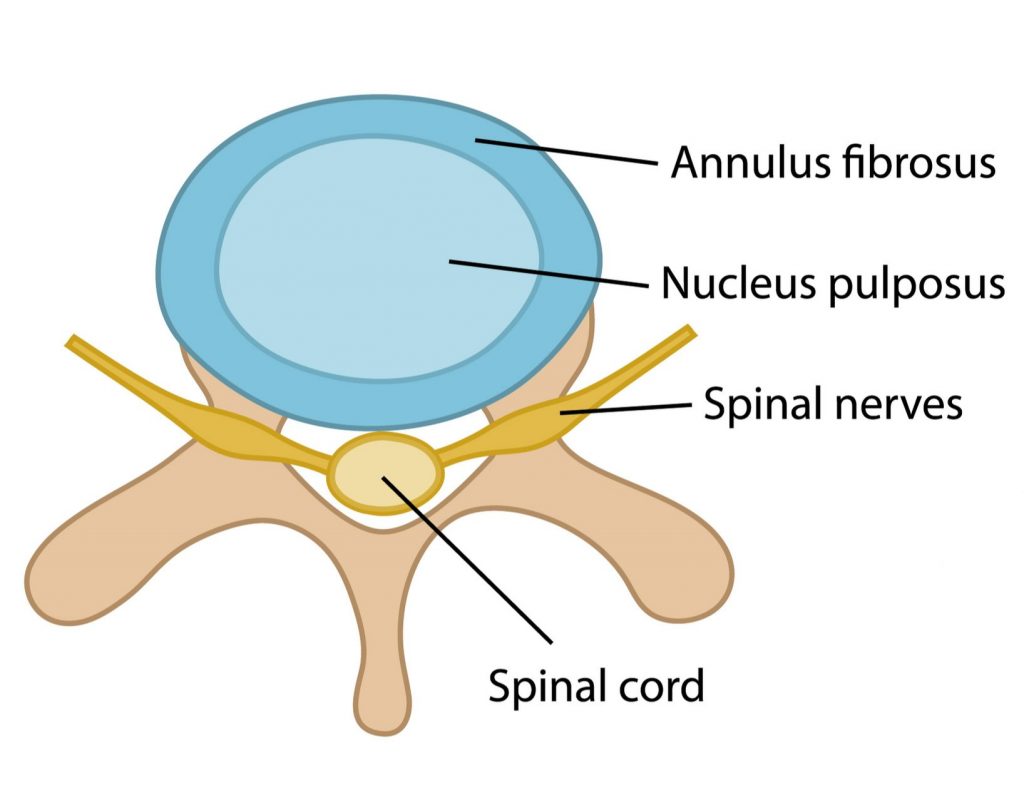
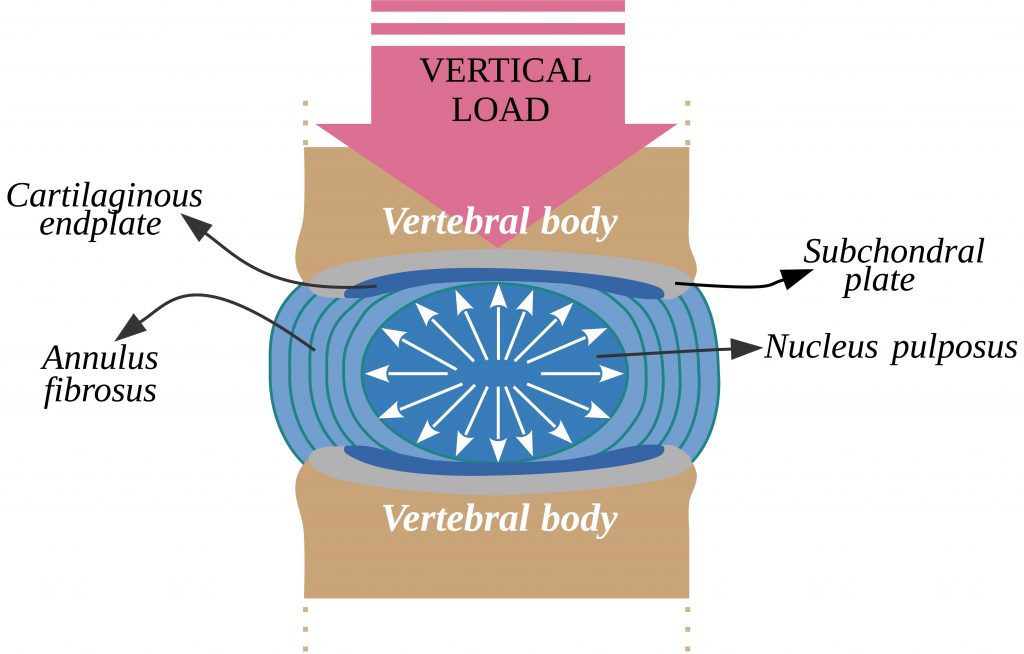
The IVD is made from strong fibrocartilage and divided into 2 sections:
- annulus – tough fibrous exterior
- nucleus – jelly-like interior
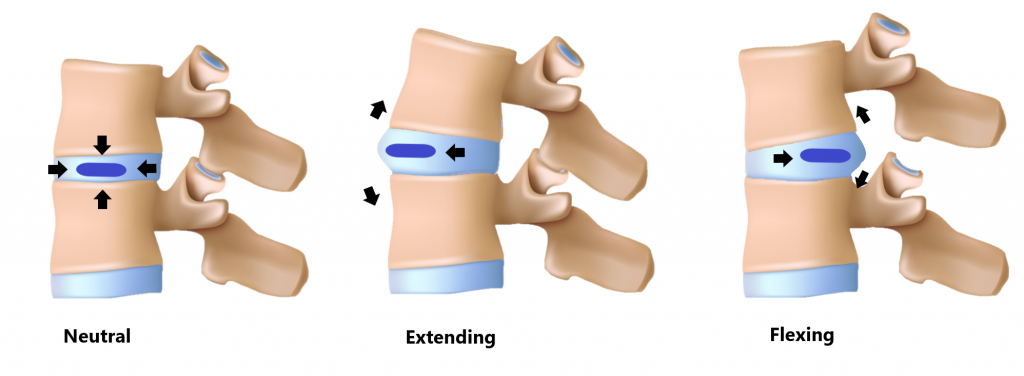
This is similar to a jelly donut, if you compress one side the contents will move in the opposite direction.
Functions of the IVD
Shock Absorption
The IVD is designed to absorb impact through the spine during activities such as running and jumping.

Withstand Compressive Loads
The IVDs are excellent at handling compressive loads (i.e. heavy lifting) PROVIDING the load is in a central position
Spacer
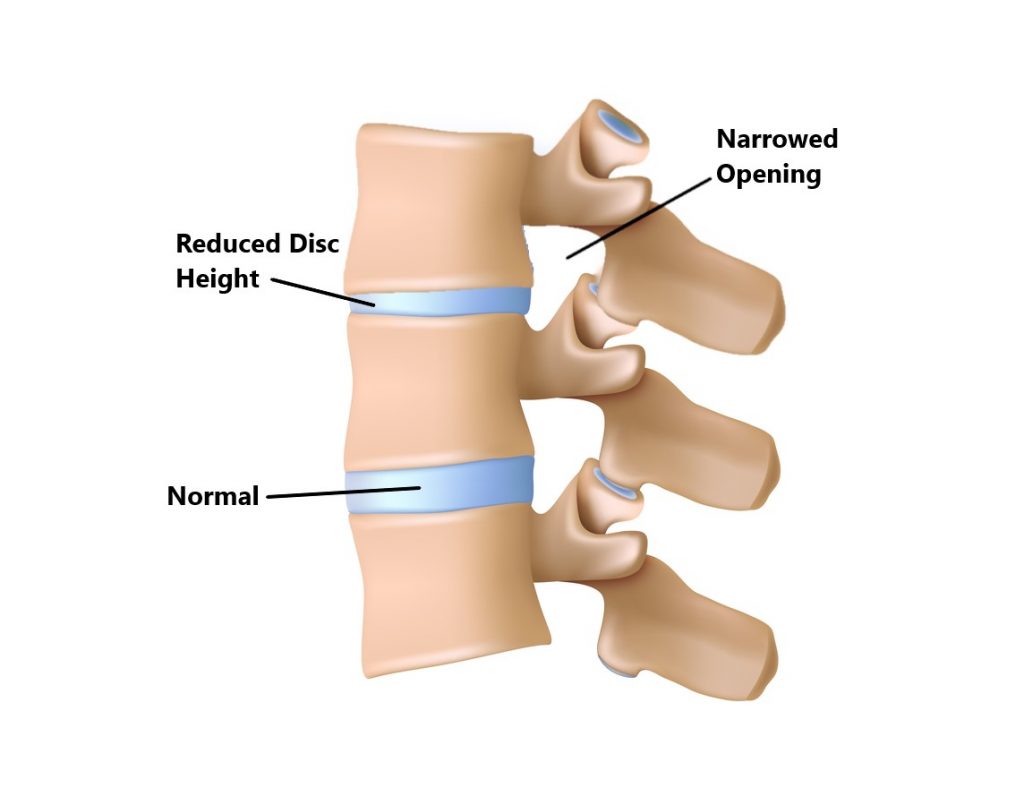
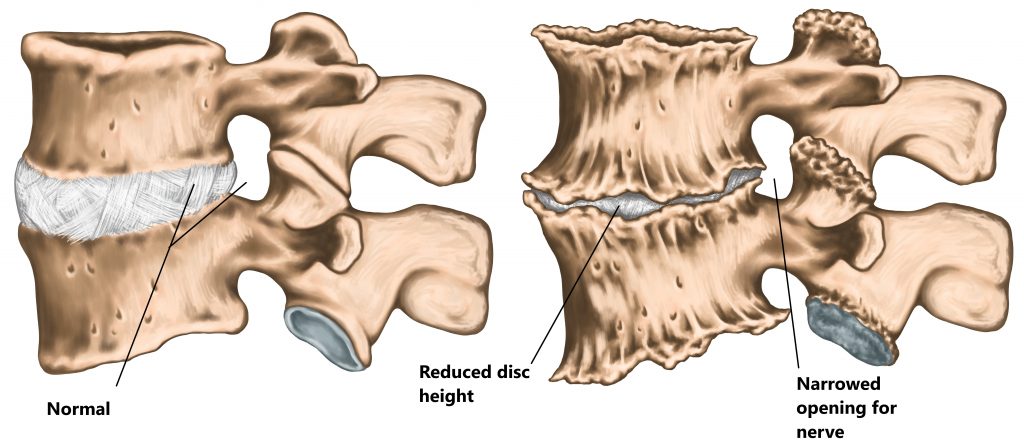
Openings formed on either side of the spine called the intervertebral foramen enable the spinal nerves to pass through. The IVDs help maintain this space between adjacent vertebrae so that the nerves do not become compressed.
Intervertebral Disc Injuries
Abnormalities of the IVD are a normal part of the ageing process and often observed in people with no symptoms. Studies have found up to 40% of people in their 20’s with no symptoms will have some kind of IVD abnormality on an MRI scan, these percentages increase as we age. Remember, it is normal to be abnormal!
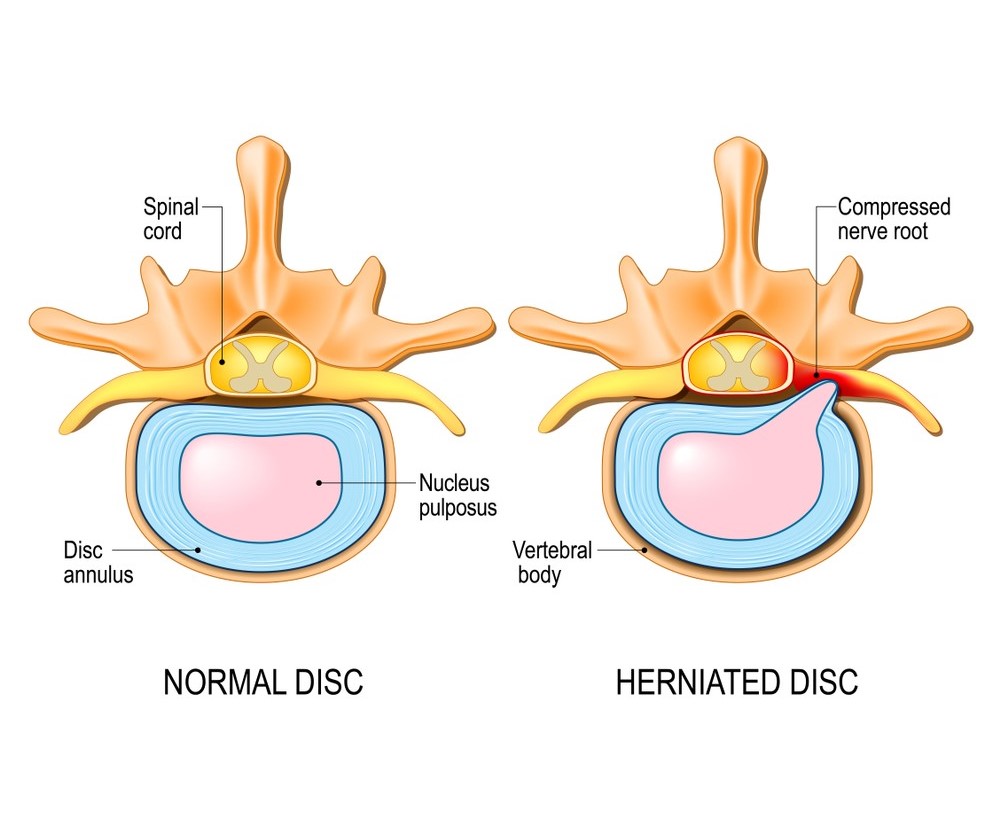
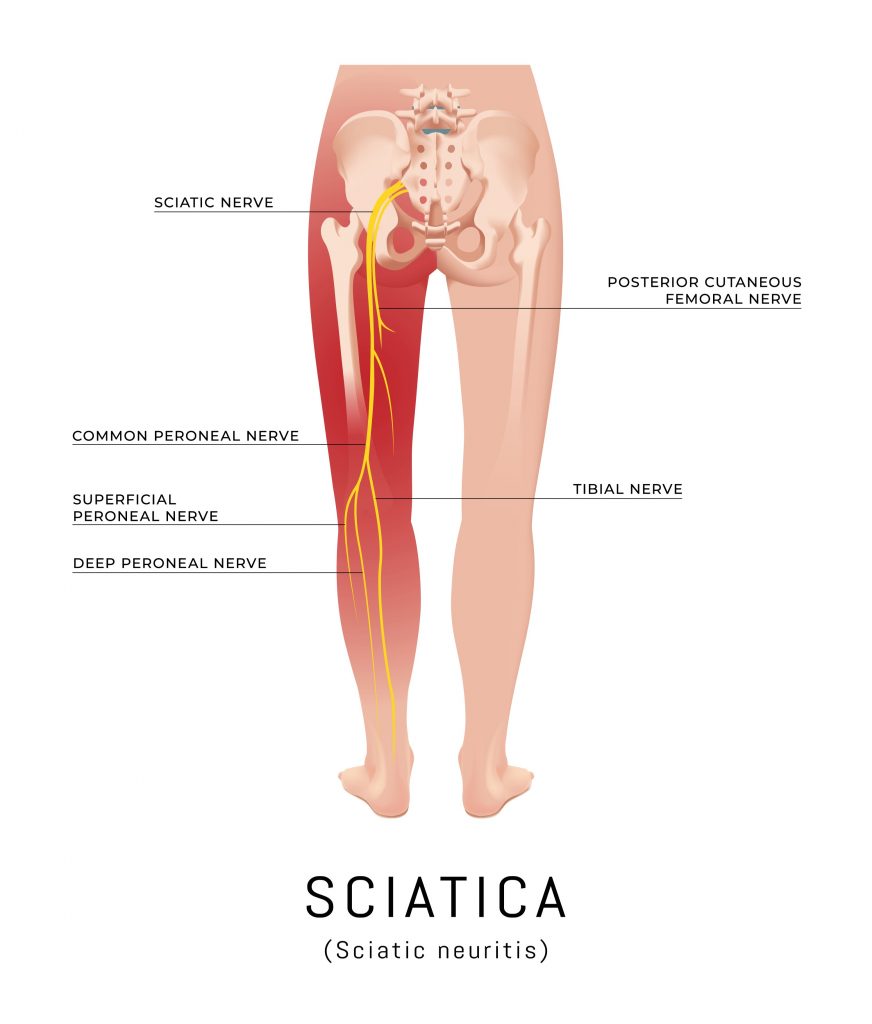
Due to the close proximity of the IVDs to the spinal nerves and spinal cord, injuries can result in irritation and/or compression of the neural structures (see image below). This can give rise to symptoms into the upper and lower limbs (i.e. weakness, pins and needles, numbness).
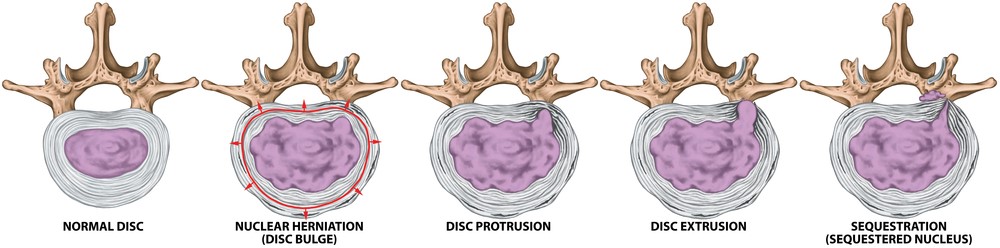
We have listed some common IVD injuries below:
Bulges/Prolapses/Slips/Herniation
These are common terms used to describe denaturing of the shape of an IVD. Damage to the annulus will give rise to a weakening of the outer wall making it easier for the inner contents to bulge out to one side.
Disc Dessication/Degeneration
This is most commonly seen in older populations. The IVD’s are made of cartilage and have a high water content. As we age our discs loose their hydration and become smaller and less flexible. This makes the IVD more prone to developing tears and bulges. As mentioned above advanced disc degeneration can lead to compression of the neural structures due to a loss of the “spacing” function.
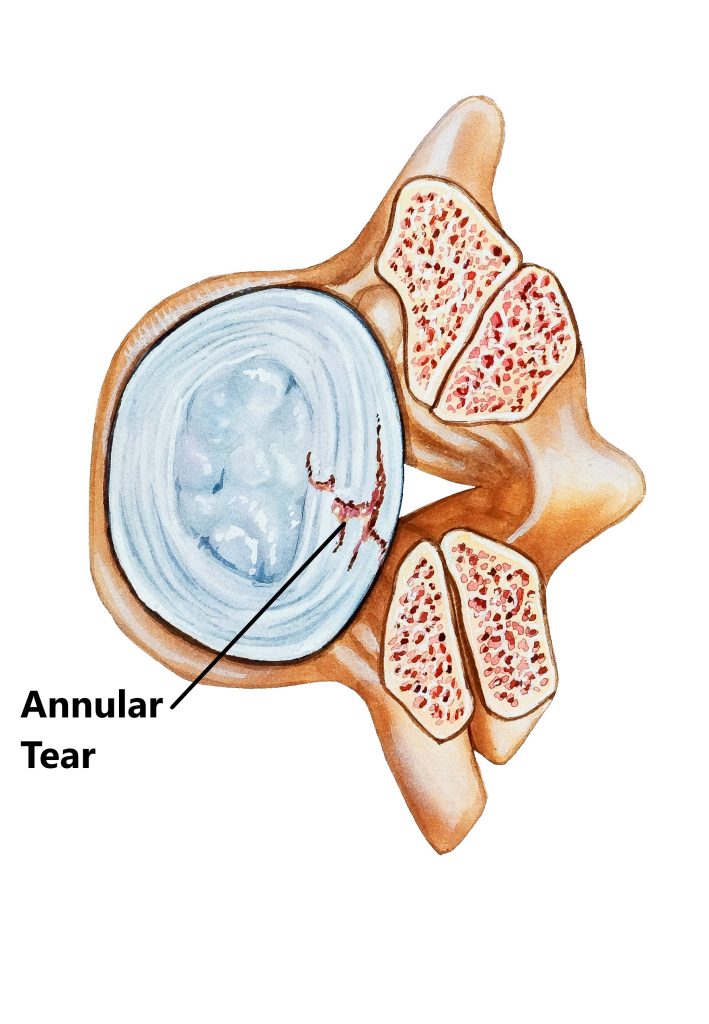
Annular Tear/Fissure
This refers to a tear to the outer wall of the IVD. The outer 1/3 of the annulus has a rich nerve supply, injuries to this area can be extremely painful without necessarily having neural symptoms.
Common Causes of Intervertebral Disc Injuries
- holding prolonged static postures
- prolonged sitting
- prolonged/repeated bending
- lifting in bent positions
- lifting and twisting
- lifting from the ground
- lifting or pulling in outstretched positions
- heavy lifting
- age related degeneration

Intervertebral Disc Injury Risk Factors
- sedentary lifestyle
- lack of physical exercise
- smoking and excessive alcohol intake
- high BMI
- stress, anxiety and depression
- physically demanding occupations
- older age

Common Symptoms of Intervertebral Disc Injuries
- localised back pain
- neural signs into the upper and lower limbs (i.e. burning, pins and needles, numbness, weakness, sensation changes)
- spinal cord signs (i.e. loss of bladder and bowel control, increasing clumsiness and weakness in the arms/legs, sudden sexual dysfunction symptoms into both arms/legs)
Common Associated Injuries
- nerve and spinal cord irritations (as discussed)
- facet joint injuries
Diagnosis of Intervertebral Disc Injuries
Diagnosing an IVD injury is based on an individuals clinical presentation and imaging. In many cases imaging is not always necessary.
- Subjective and Physical Examination
- Xray
- CT
- MRI

Management
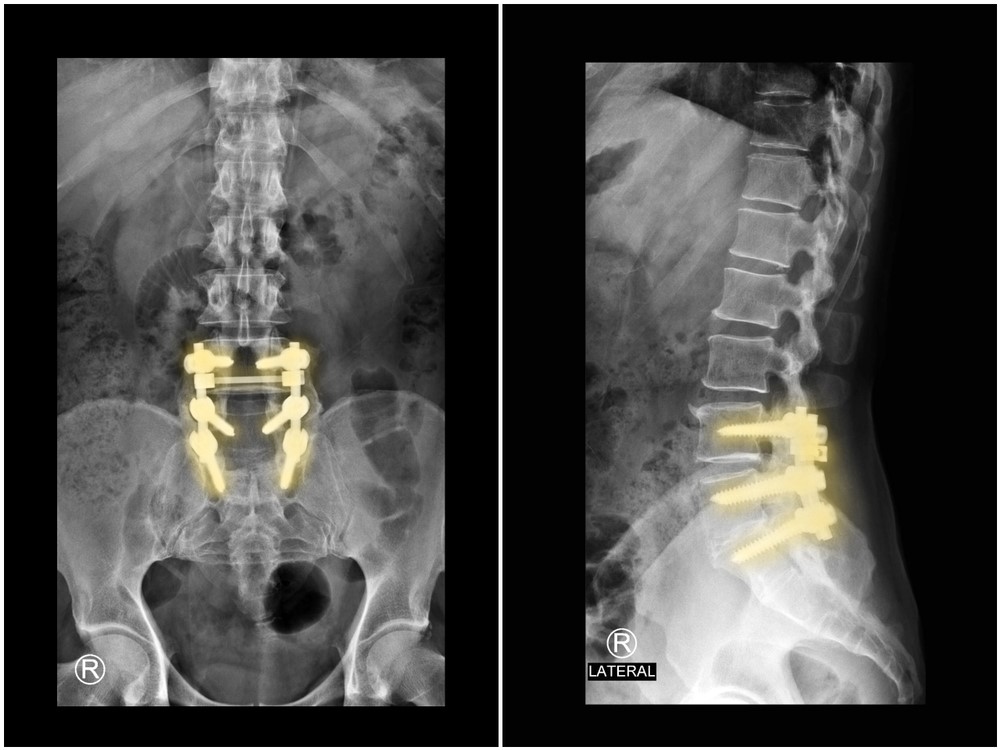
IVD injuries are typically managed with conservative physiotherapy treatment. Occasionally a cortisone injection may be required to alleviate inflammation. More severe cases may require surgery to decompress the spinal nerves however, this only constitutes a small percentage.
Physiotherapy Management
- Following an acute injury our priority is to minimise the extent of damage, reduce inflammation and decrease pain. Modalities such as RICE (Rest, Ice, Compression, Elevation), strapping, manual therapy and acupuncture may be used
- Provide education regarding the injury, address unhelpful beliefs, identify and modify aggravating factors
- Restore pain free range of motion and return to basic activities. Commence gentle stretches and a walking program
- Restore strength of the core and lower limbs. Commence a graded strengthening program.
- Identify and address aggravating factors, movement and postural issues that may have contributed to the injury.
- Graded return to work, sport and function.

Red Flags!
These are signs and symptoms of more serious causes and require urgent medical review:
- spinal cord signs (as above)
- symptoms are also associated with a lack of balance and changes in gait pattern
- onset of symptoms following trauma (i.e. fall, car accident)
- If you get also get symptoms at night that does not change with activity

Please keep in mind the information provided is general in nature and should not be used as a substitute to consult your treating health professional. If you have any specific questions or require assistance with your individual treatment requirements please do not hesitate to contact MyFamily Physio Mona Vale, Northern Beaches Sydney.
Related Injuries