Articles Ankle Sprains
The ankle ligaments are the most commonly sprained ligaments in your body. Please continue reading to get a better understanding of the different types of ankle sprains, risk factors, indications for Xray imaging and physiotherapy management.
Basic Anatomy
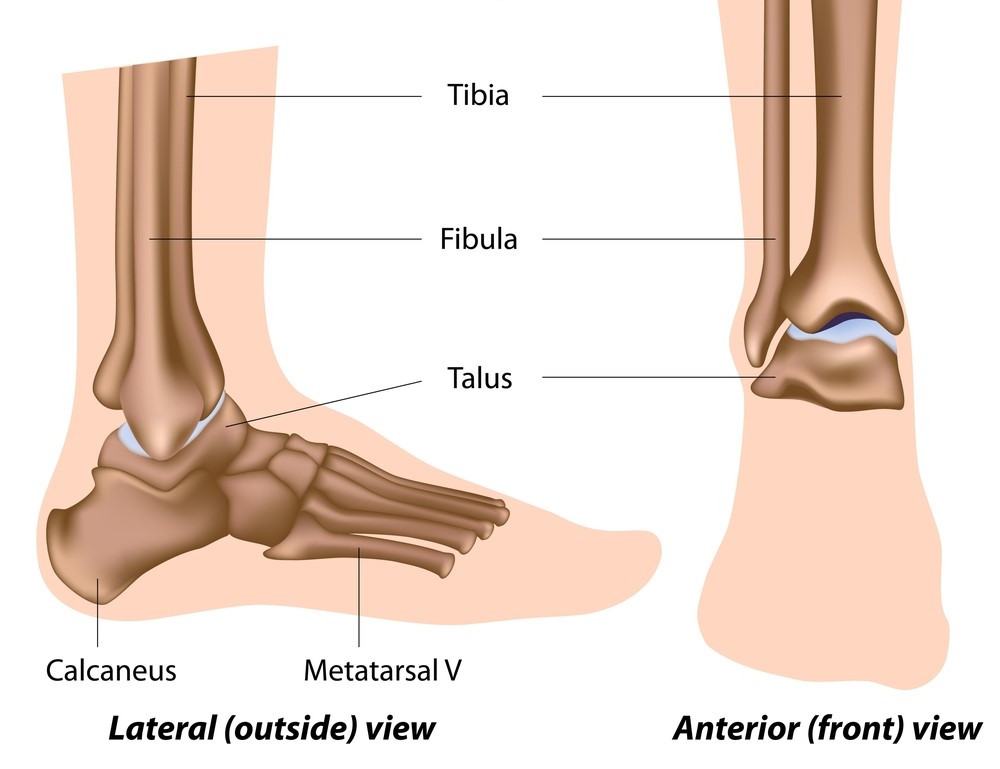
Your ankle joint is formed by 3 bones:
- tibia (inside lower leg bone)
- fibula (outside lower leg bone)
- talus (foot bone)
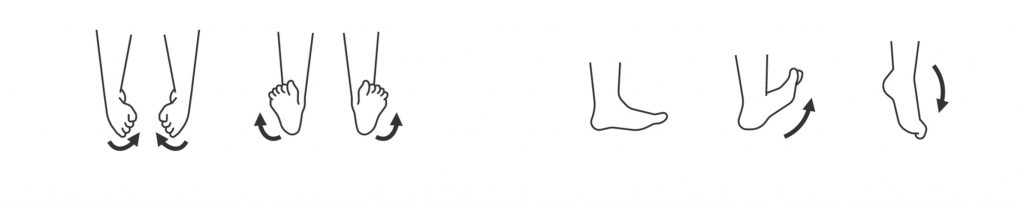
Nature has designed your ankle joint so that it can move specific directions:
- toe up and down (dorsiflexion/plantarflexion)
- side to side (inversion/eversion)
Ligaments connect your bones together to prevent excessive movement. Your ankle joint has 3 groups of ligaments:
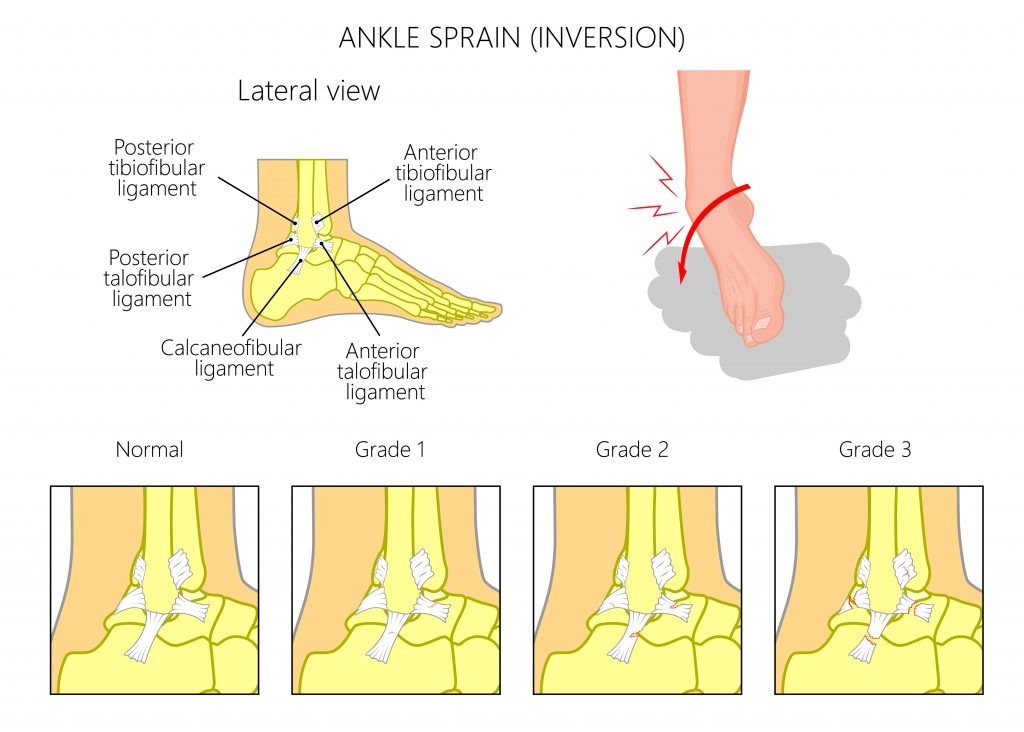
Lateral Ligaments, are formed on the outside of your ankle joint to prevent excessive rolling inwards movements.
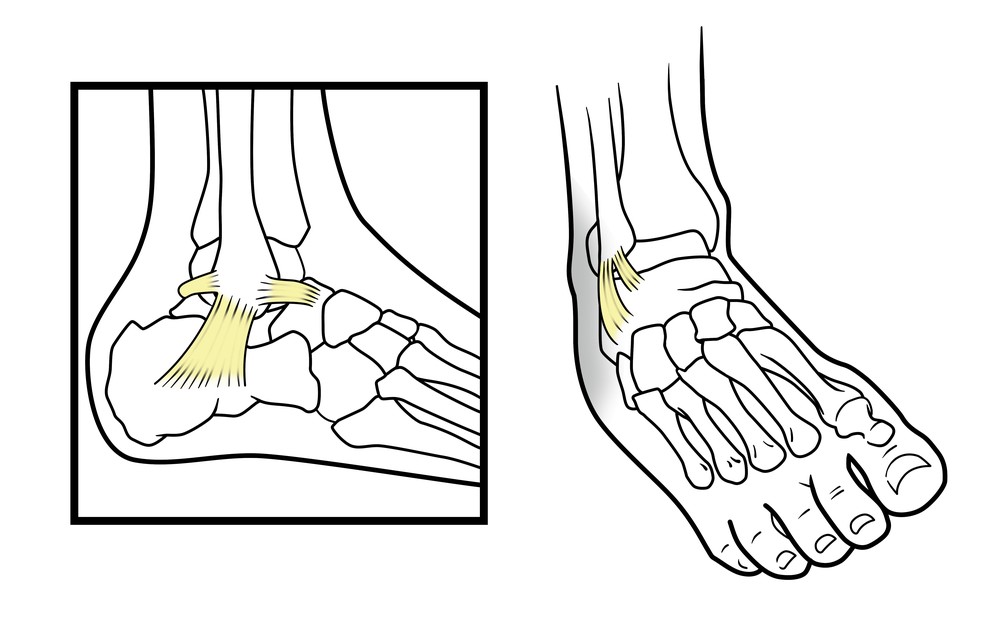
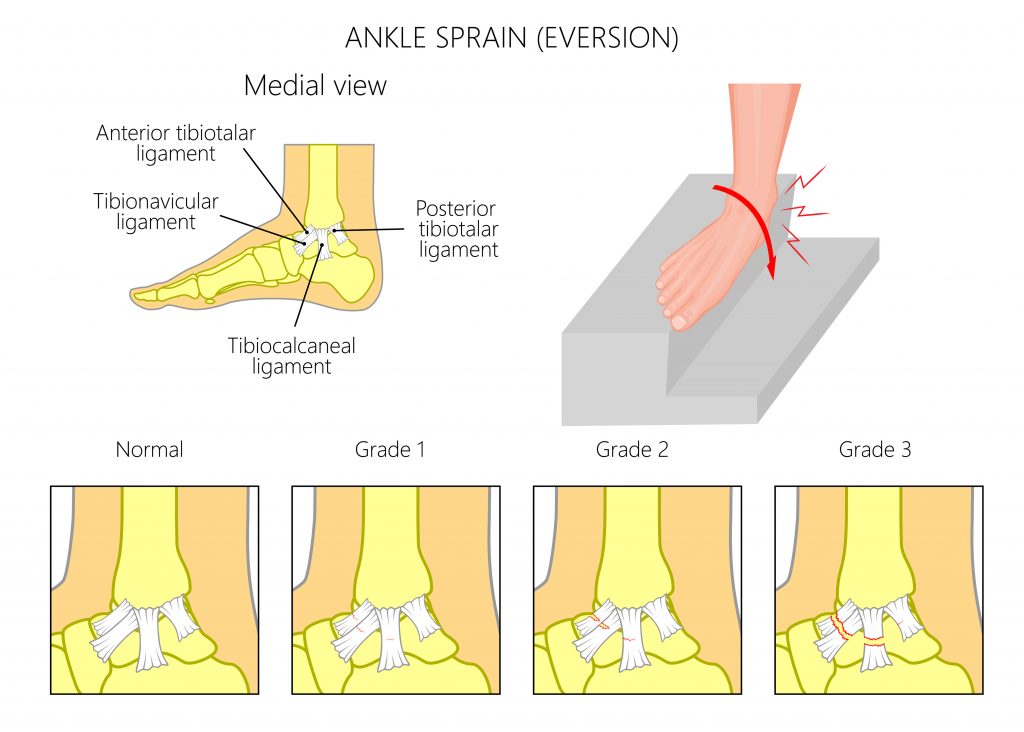
Medial Ligaments, are formed on the inside of your ankle joint to prevent excessive rolling outwards movements.

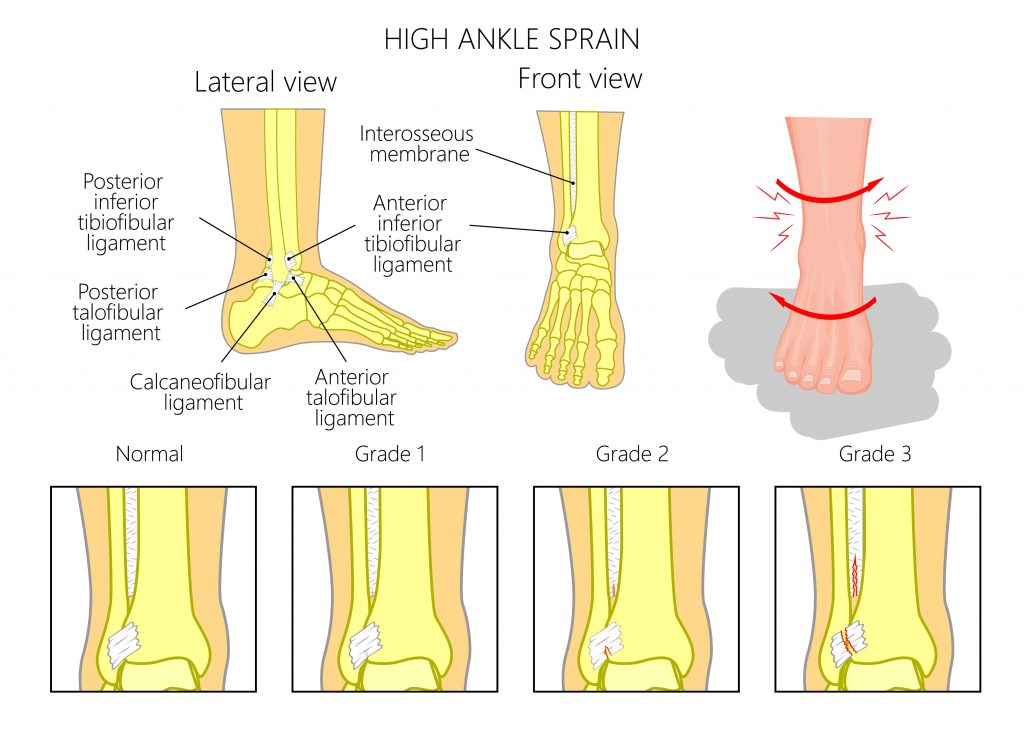
High Ankle Ligaments, are formed between your lower leg bones to prevent them from separating.

What is an Ankle Sprain?
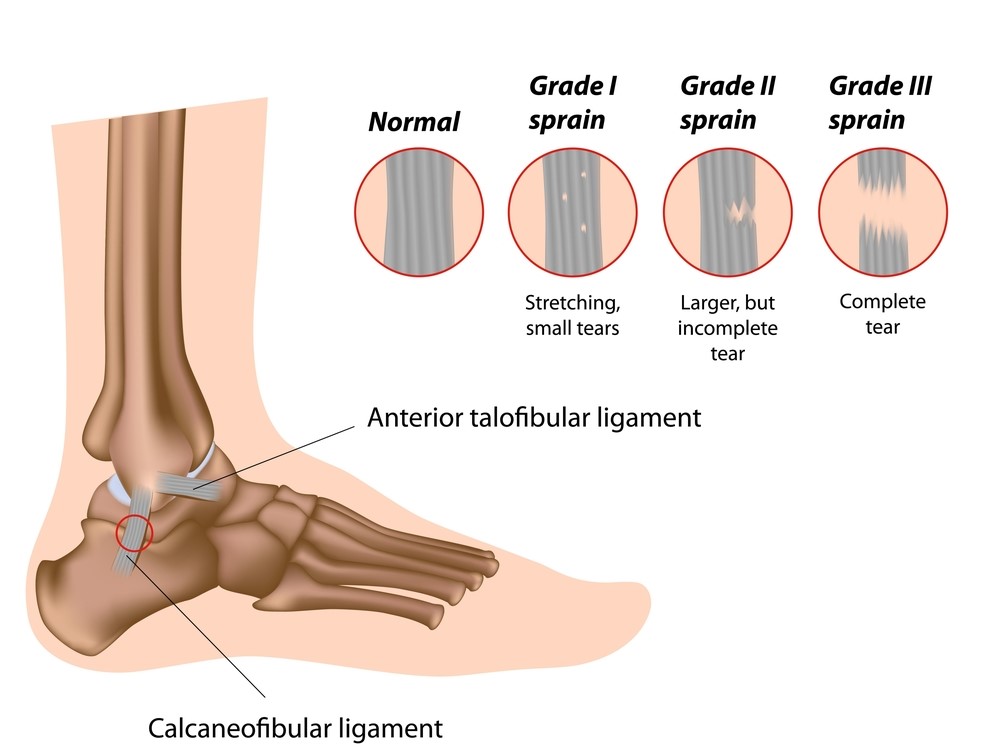
An ankle sprain arises when a ligament is over stretched beyond its normal limits resulting in a tear to the tissue. This is similar to over stretching a rubber band, if you go too far it will eventually snap. Ankle sprains are typically graded from 1 (minor) – 3 (complete rupture).
What are the Different Types of Ankle Sprains?
Low grade ankle sprains are typically managed with conservative physiotherapy treatment. Higher grade sprains and injuries involving fractures should be reviewed by your doctor/specialist.
Lateral Ankle Sprains
These are by far the most common and account for approximately 85% of all ankle sprains. This is due to the shape of the joint surfaces allowing more movement to occur when the sole your foot is turned inwards compared to turning out. In these instances the lateral ligaments are sprained following a sudden incident where the ankle rolls inwards forcing you to land heavily on the outside boarder of your foot (i.e. stepping off a kerb).
Medial Ankle Sprains
Less common are medial ankle sprains. This is due to the shape of the joint surfaces being more restrictive in this direction and also the medial ligaments being a lot stronger. In these instances the medial ligaments are sprained following a sudden incident where the ankle rolls outwards forcing you to land heavily on the inside boarder of your foot.
High Ankle Sprains (Syndesmosis Injury)
High ankle sprains account for approximately 1% of all ankle sprains. In these situations the high ankle ligaments are over stretched, resulting in the lower leg bones being pulled apart and separating.
These injuries typically occur following an incident where an individual’s knee is suddenly turned inwards while weight bearing through their foot (i.e. getting tackled from the side) or where the ankle is forcefully pushed into a “toe up” position (i.e. another player landing heavily on the back of your calf).
A lot more force is required to sprain the high ankle ligaments. Therefore, these injuries generally take longer to heal and are often associated with fractures. Unlike medial and lateral sprains, these injuries often lack the presence of visible inflammation and swelling.
Chronic/Recurrent Ankle Sprains
Inadequate rehabilitation often gives rise to recurrent ankle sprains. It is very important to regain your strength, mobility and balance otherwise, it puts you at an increase risk of reinjury. Recurrent sprains will weaken and overstretch the ligaments and can eventually give rise to complete ligament ruptures, cartilage injuries, fractures and an early onset of osteoarthritis. Chronic ankle sprains may require an orthopaedic opinion as surgery may be required.
What are the Signs and Symptoms of an Ankle Sprain?
- sudden acute onset of ankle pain following trauma
- signs of inflammation (swelling, redness, heat, pain)
- restricted ankle movement
- pain and tenderness over the injured ligament
- difficulty/inability to weight bear
- lack of confidence walking on uneven ground due to instability
- lack of balance
- difficultly pivoting
- difficulty squatting
- difficulty standing on tip toes

Risk Factors
- history of ankle sprains
- poor rehabilitation following previous ankle sprains
- individuals who participate in sports requiring sudden changes in direction
- older athletes
- individuals with poor balance
- individuals with hyper mobile joints
- lack of ankle flexibility
- wearing inappropriate or poor fitting foot wear ( i.e. high heels)
- negotiating uneven ground

Common Associated Injuries
- fractures
- cartilage damage
- peroneal tendon injuries
- osteoarthritis

Diagnosis
Diagnosing an ankle sprain is mainly based on an individuals clinical presentation. Imaging my be required to detect fractures, higher grade tears, cartilage and tendon injuries. In many cases imaging is not always necessary.
- Subjective Examination
- Physical Examination
- Xray
- Ultrasound
- CT
- MRI

Should I Get an Xray?
As a general guide an Xray will be required when:
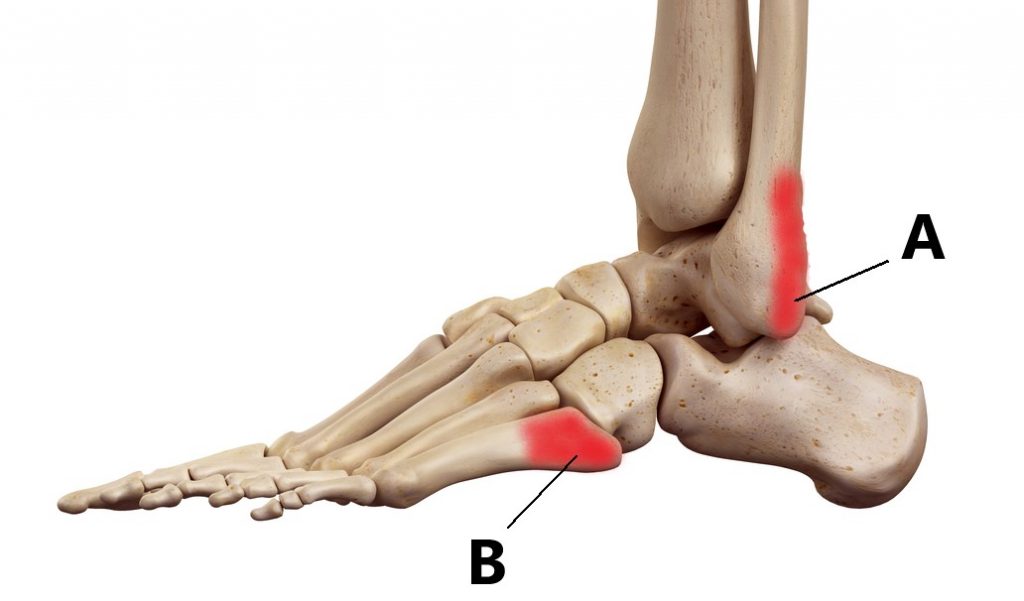
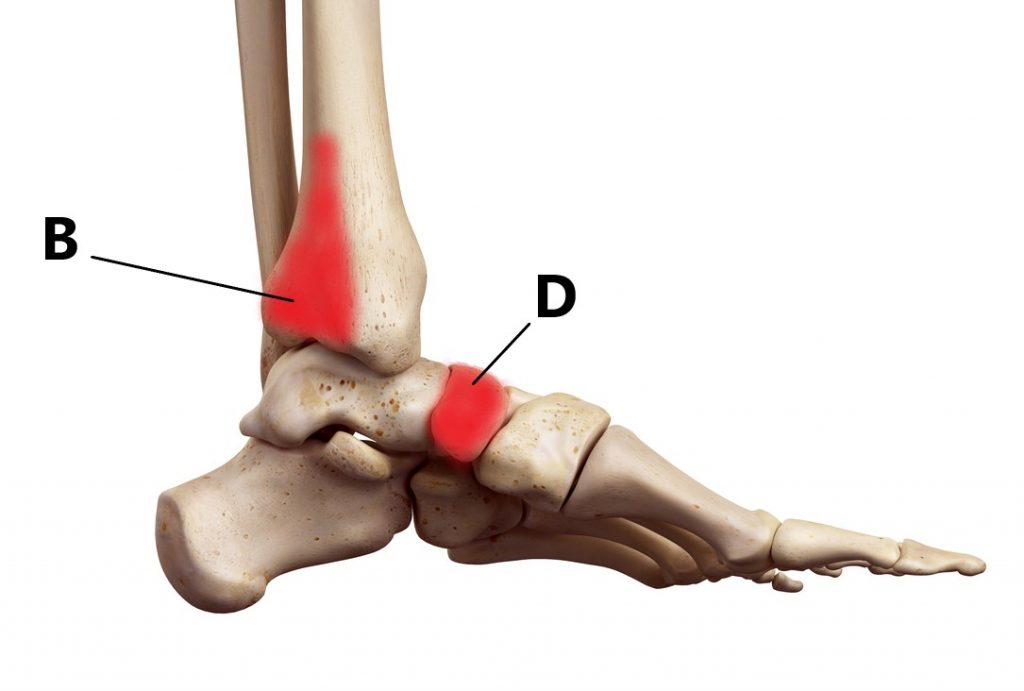
- Bone tenderness over A or C (outside of ankle) OR
- Bone tenderness over B or D (inside of ankle) OR
- Inability to weight bear immediately following AND 1 hour after the initial injury
What Happens if I Have a Fracture?
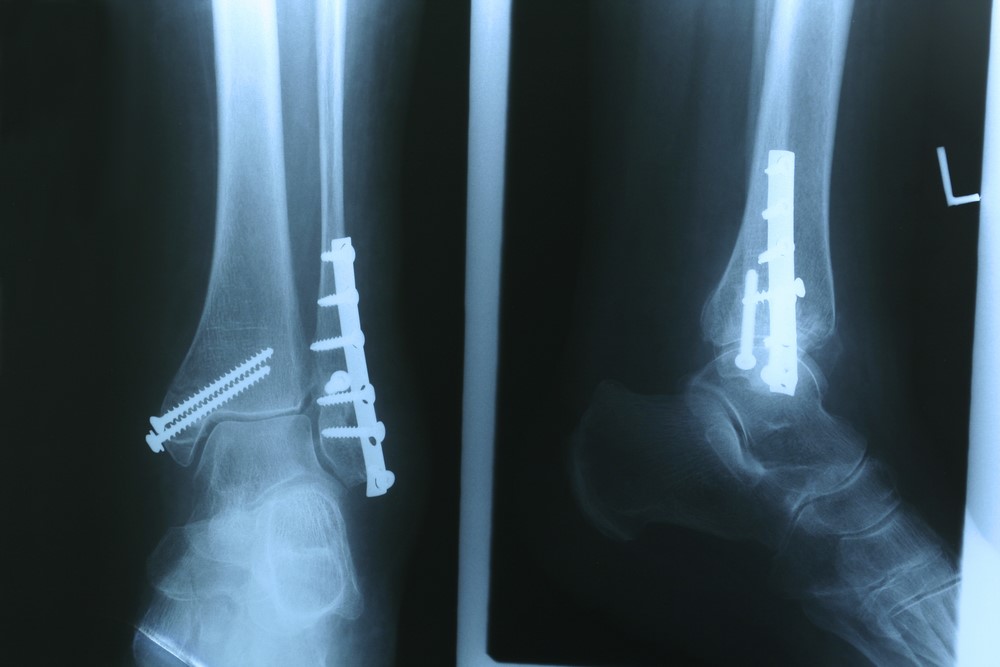
Fractures are managed depending on their size, location, position and stability. Larger fractures, fractures involving the joint surfaces, displaced fractures and unstable fractures will require an orthopaedic opinion as surgery may be required.
Smaller, non-displaced stable fractures are typically managed by immobilising your ankle in a boot for several weeks to enable bone healing before commencing physiotherapy treatment.
Your treating doctor should provide you with specific instructions, important things to find out include:
- Am I allowed to weight bear on my foot?
- How much weight am I allowed to put through my foot?
- How long do I need to be in the boot?
- When can I commence physiotherapy treatment?

Physiotherapy Management
Ankle sprains are typically managed with conservative physiotherapy treatment.
- Following an acute injury our priority is to minimise the extent of damage, reduce inflammation and decrease pain. Modalities such as RICE (Rest, Ice, Compression, Elevation), strapping, protective bracing and manual therapy may be used.
- Provide education, address unhelpful beliefs regarding the injury (i.e. walking will not cause more damage), identify and modify aggravating factors
- Normalise gait pattern (i.e. don’t walk on your tip toe, put your heel down!)
- Restore pain free ankle range of motion and prevent secondary complications (i.e. ankle and calf stiffening).
- Strengthening of the ankle muscles
- Balance retraining
- Identify and address movement and postural issues that may have contributed to the injury
- Graded return to work, sport and function.
Please keep in mind the information provided is general in nature and should not be used as a substitute to consult your treating health professional. If you have any specific questions or require assistance with your individual treatment requirements please do not hesitate to contact My Family Physio in Pittwater Place Shopping Centre, Mona Vale.
Related Articles