Articles Achilles Tendon Injuries
This article discusses different types of Achilles tendon injuries, symptoms, risk factors and management. Please continue reading to learn more.
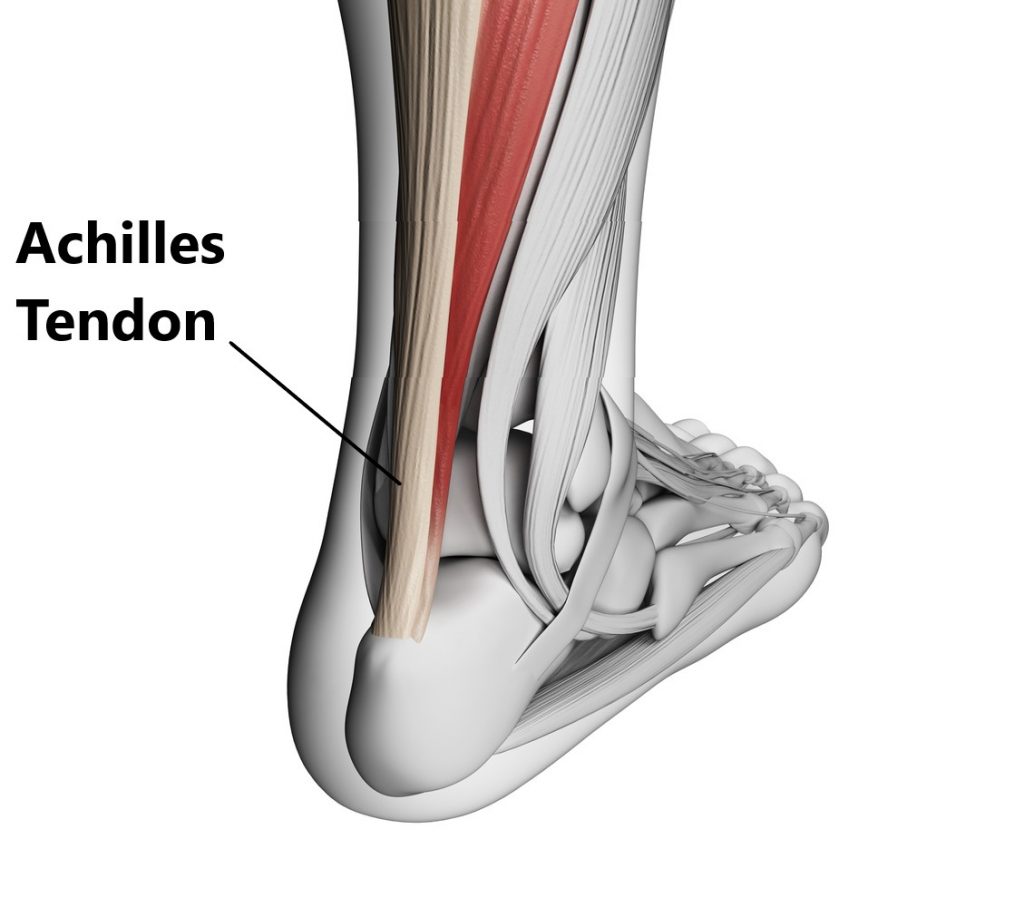
Basic Anatomy
Tendons connect muscles to bones, they are comprised of collagen fibres and are designed to withstand tension. The largest tendon in your body is the Achilles tendon. At the back of your lower leg the Achilles tendon connects your calf muscle to your heel bone.
What Do Your Achilles Tendons Do?
Your Achilles tendons have 2 actions:
- enables the “tip toe” movement at the ankle
- controls the descent from standing on your tip toes to lowering your heels to the ground

In functional terms, your Achilles tendons allow you to:
- propel your body forwards during walking and running

- jump

- stand on your tip toes

- prevents you from falling flat on your face when standing, walking and running
- absorb shock when landing

Achilles Tendon Injuries
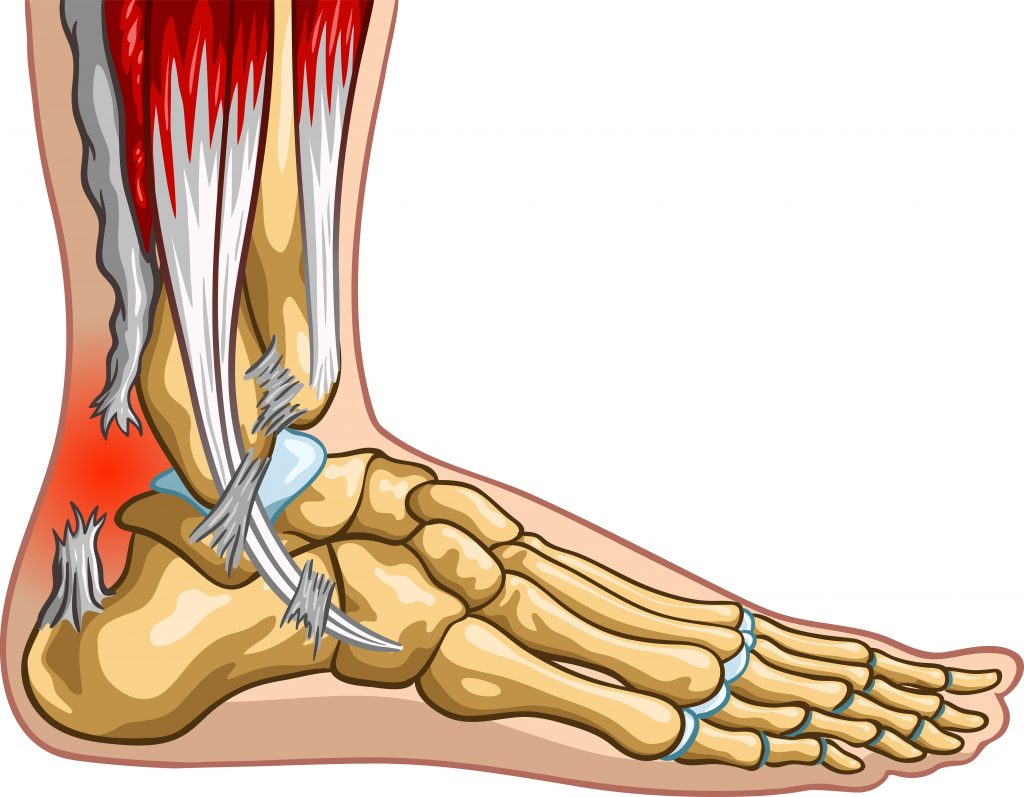
Unfortunately, tendons lack a good blood supply, this is why they appear white. This makes them slow healers taking several months to recover at best.
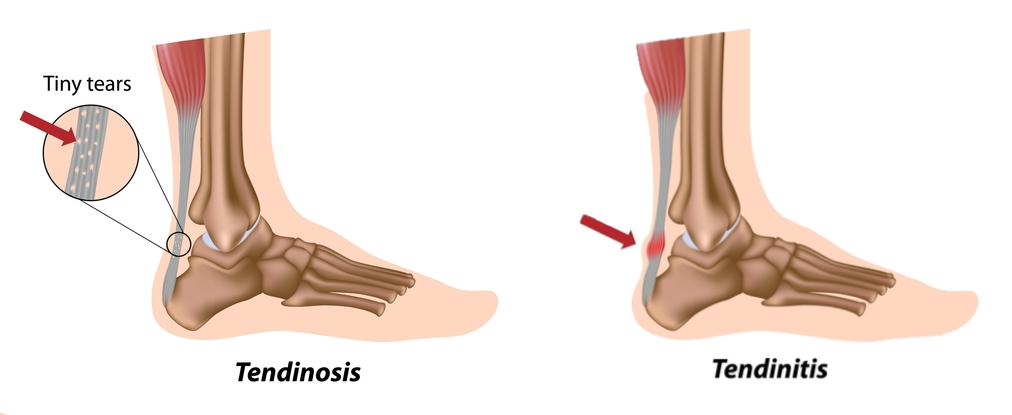
Achilles Tendinopathy/Tendinitis
This refers to irritation of the Achilles which leads to micro tears and thinning of the tendon. Occasionally, these injures arise from acute trauma (i.e. hard blow to the back of the Achilles), but more commonly develop over a period of time as a result of overuse. The most important aspect of treatment in managing this condition is to prevent further aggravations by adequately resting the tendon. This may involve reducing your amount of weight bearing activity, modifying your footwear (i.e. orthotics, heel raise) or unloading the tendon (i.e. taping).
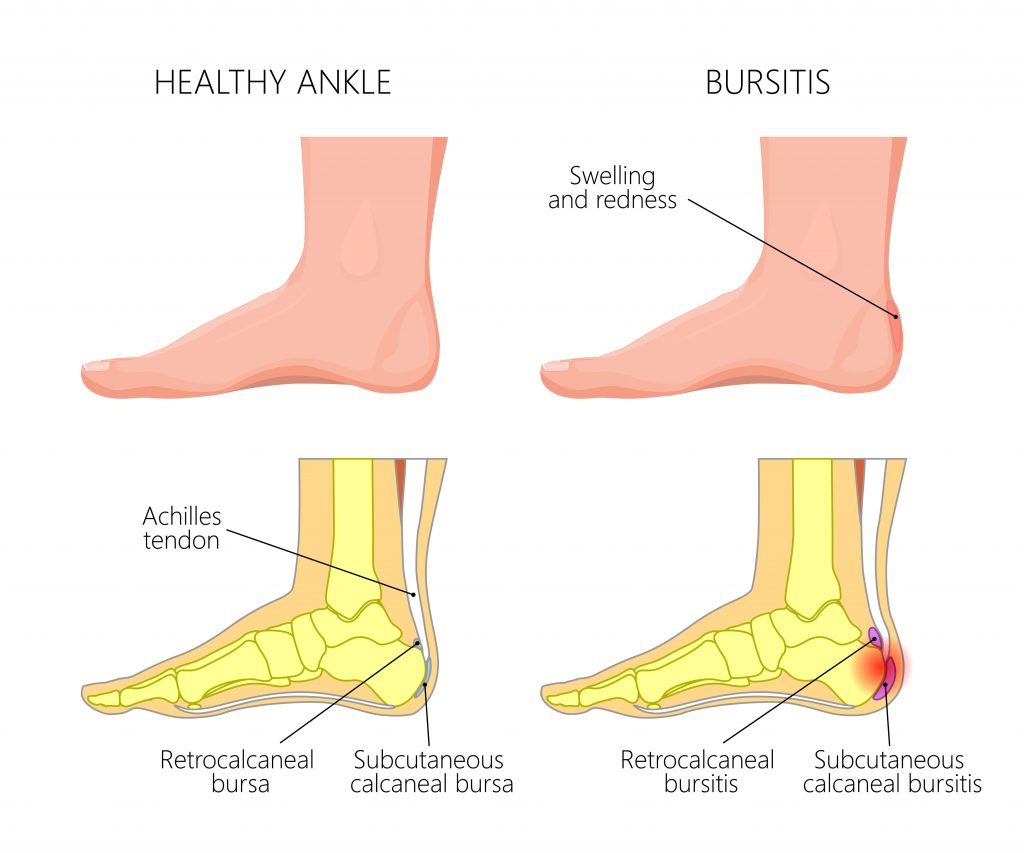
Achilles Bursitis
A bursa is a fluid filled sac found in areas of the body where a tendon or muscle rubs over a bone. The function of a bursa is to decrease the amount of friction, if the bursa becomes inflamed it can swell causing compression and pain in the surrounding anatomical structures. Close to where the Achilles tendon inserts onto the heel bone are 2 bursae. It can be difficult to distinguish between an Achilles tendinopathy and bursitis as the symptoms are essentially identical, the good news is the management is also very similar.
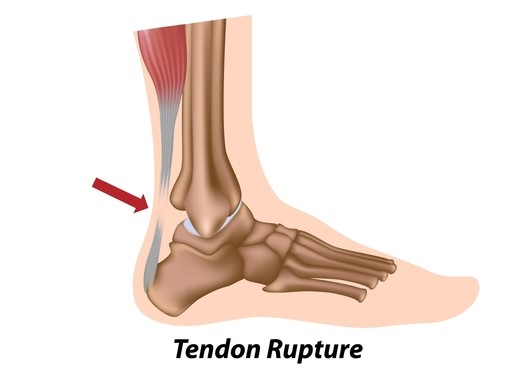
Achilles Tears and Complete Ruptures
Achilles tears and ruptures typically occur as a result of suddenly “taking off ” on the affected leg (i.e. suddenly sprinting, jumping, changing direction). People normally report hearing an audible ‘pop’ or feel as if someone had thrown a cricket ball at the back of their leg. Large tears and complete ruptures will likely require surgical repair.
Symptoms
Achilles Tendinopathy/Bursitis
- swelling and thickening of the tendon
- weakness
- stiffness and pain first thing in the morning that improves as you warm up
- redness, heat and swelling
- increased pain after activity

Achilles Tears and Complete Ruptures
- feeling a “pop’ at the time of injury
- having a palpable divot in the Achilles tendon
- inability to point toe
- inability to walk
Risk Factors For Achillies Tendon Injuries
- obesity
- male gender, 40-50 years of age (especially for Achilles tears and ruptures )
- distance running
- participating in sports involving sprinting and jumping
- weak calf muscles
- stiff ankle joints
- occupations requiring prolonged standing
- flat feet
- over training or sudden increases in activity (i.e. additional practice sessions for sport)
- wearing unsupportive foot wear
- sudden change in terrain (i.e. walking on hills, running on concrete)
- commencing unaccustomed activity (i.e starting a new fitness regeime)

Diagnosis
Diagnosing Achilles tendon injuries are mainly based on an individual’s clinical presentation. In many cases imaging is not always necessary.
- Subjective and Physical Examination
- Ultrasound
- MRI

Management
Achilles Tendinopathy/ Bursitis
This condition is typically managed with conservative physiotherapy treatment. Anti inflammatory medications and nitrate patches may also be used to assist recovery. Cortisone injections are generally not administered to the Achilles region due to the risk of complete rupture.

Large Tears and Complete Ruptures
These generally require surgical repair followed by a period of immobilisation in a cast for approximately 6-12 weeks. It is important to commence physiotherapy treatment as soon as you are cleared by your surgeon to regain your movement and strength.

Physiotherapy Management
- Following an acute injury our priority is to minimise the extent of damage, reduce inflammation and decrease pain. Modalities such as RICE (Rest, Ice, Compression, Elevation), strapping, insertion of a heel raise and manual therapy may be used.
- Provide education, address unhelpful beliefs regarding the injury, identify and modify aggravating factors (this normally involves reducing the amount of weight bearing activities), correction of training practices, correction of foot wear issues
- Normalise gait pattern (i.e. don’t walk on your tip toes, put your heel down!)
- Restore flexibility and pain free ankle range of motion and prevent secondary complications (i.e. ankle and calf stiffening).
- Strengthening of the ankle muscles
- Balance retraining
- Identify and address movement and postural issues that may have contributed to the injury (i.e. orthotics for flat feet)
- Graded return to work, sport and function.

Please keep in mind the information provided is general in nature and should not be used as a substitute to consult your treating health professional. If you have any specific questions or require assistance with your individual treatment requirements please do not hesitate to contact MyFamily Physio on Mona Vale, Sydney.
Relevant Articles