Articles Sciatica
This article explains the basic anatomy of the spine and sciatic nerve, causes of sciatica, common symptoms, risk factors and physiotherapy management.
Basic Anatomy
The spinal column is made up of individual bones called vertebrae and named accordingly to their position in the spine (see below). The spine is divided into 4 sections:
- Cervical spine (neck) C1-C7
- Thoracic spine (upper back) T1-12
- Lumbar spine (lower back) L1-5
- Sacrum (pelvic area) S1
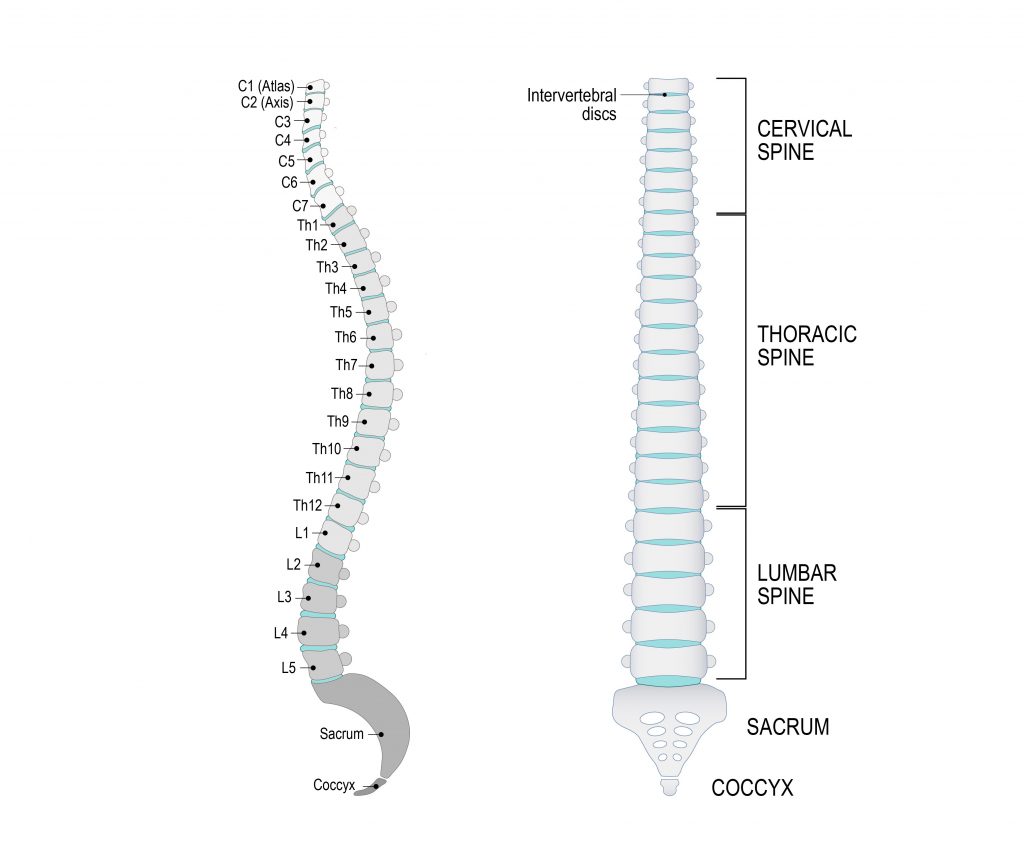
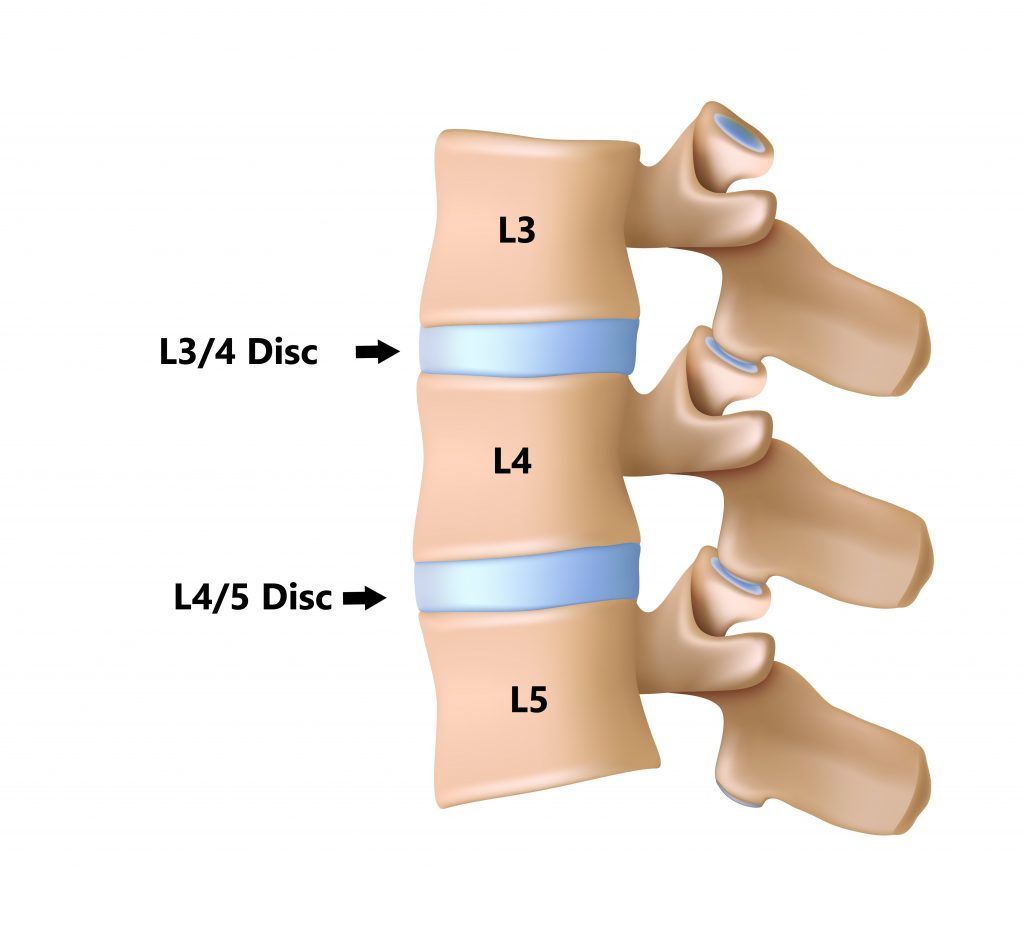
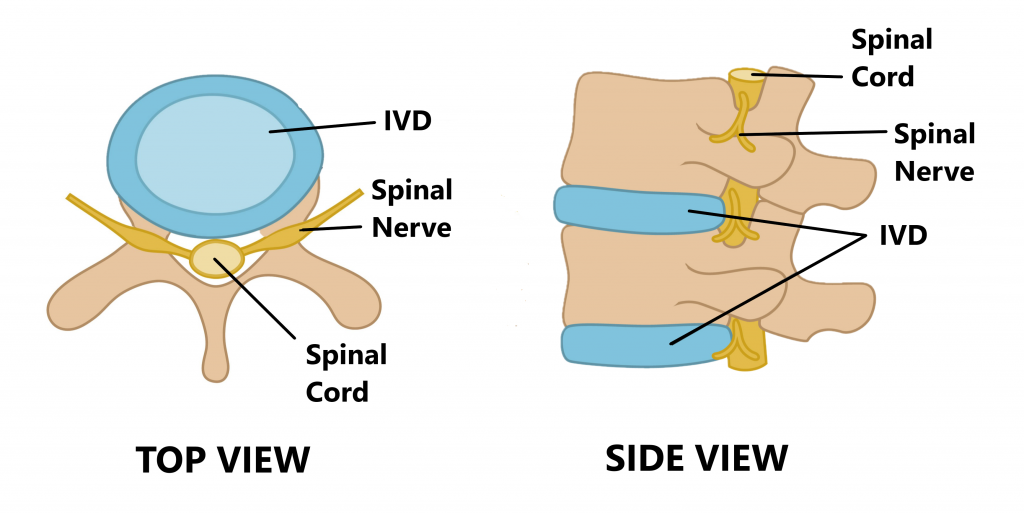
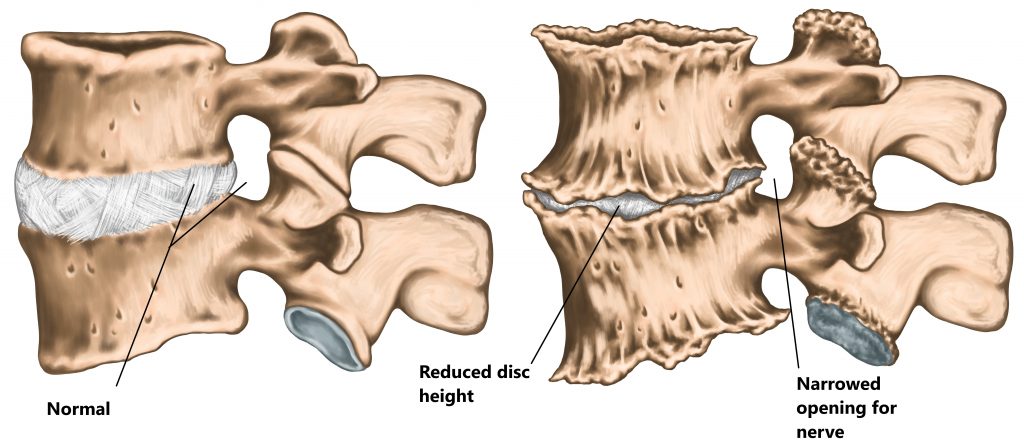
Between each vertebrae is an intervertebral disc (IVD). Each IVD is named relative to the vertebrae they sit between (see below).
Inside your spinal column sits your spinal cord where it is safely protected.
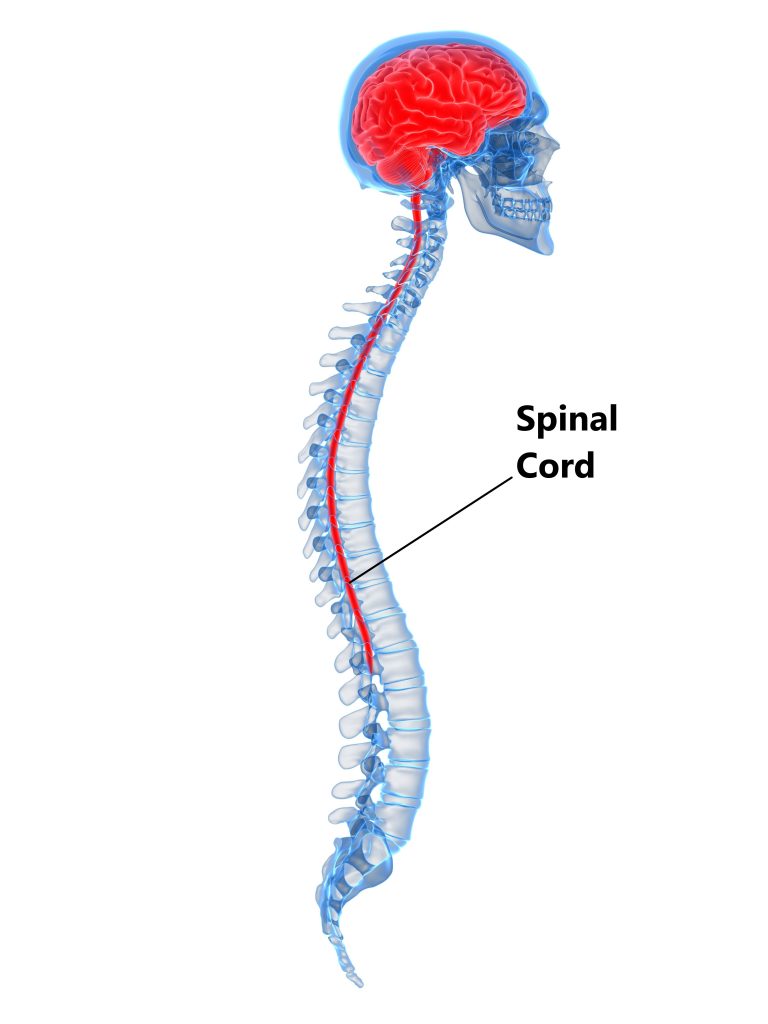
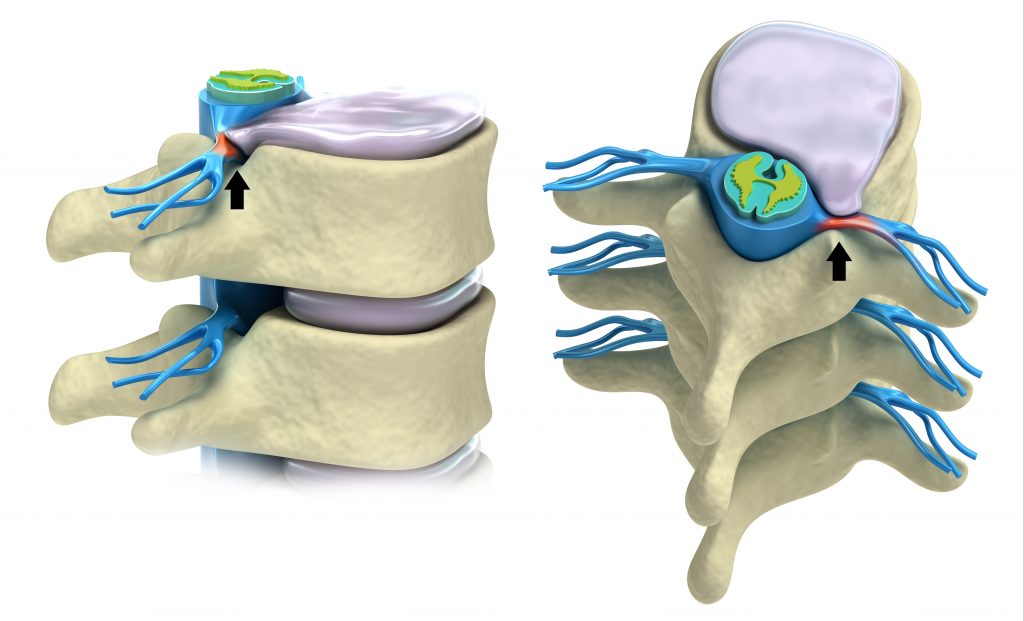
At each IVD, spinal nerves branch off the spinal cord on the left and right hand sides through openings formed between each adjacent vertebrae.
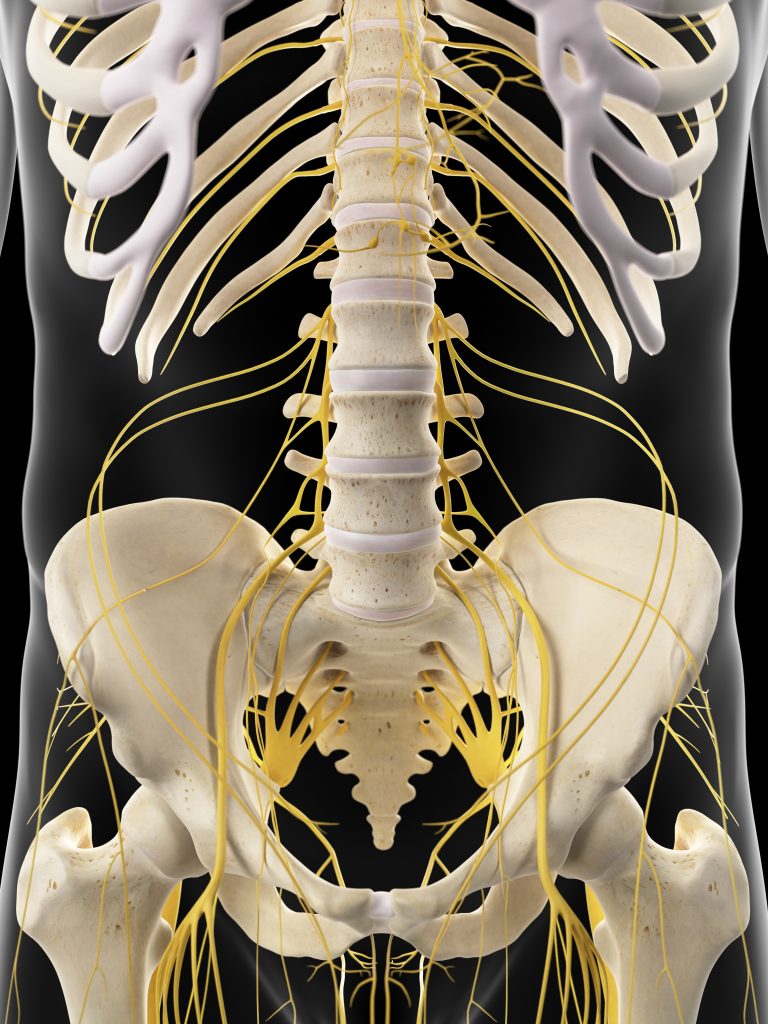
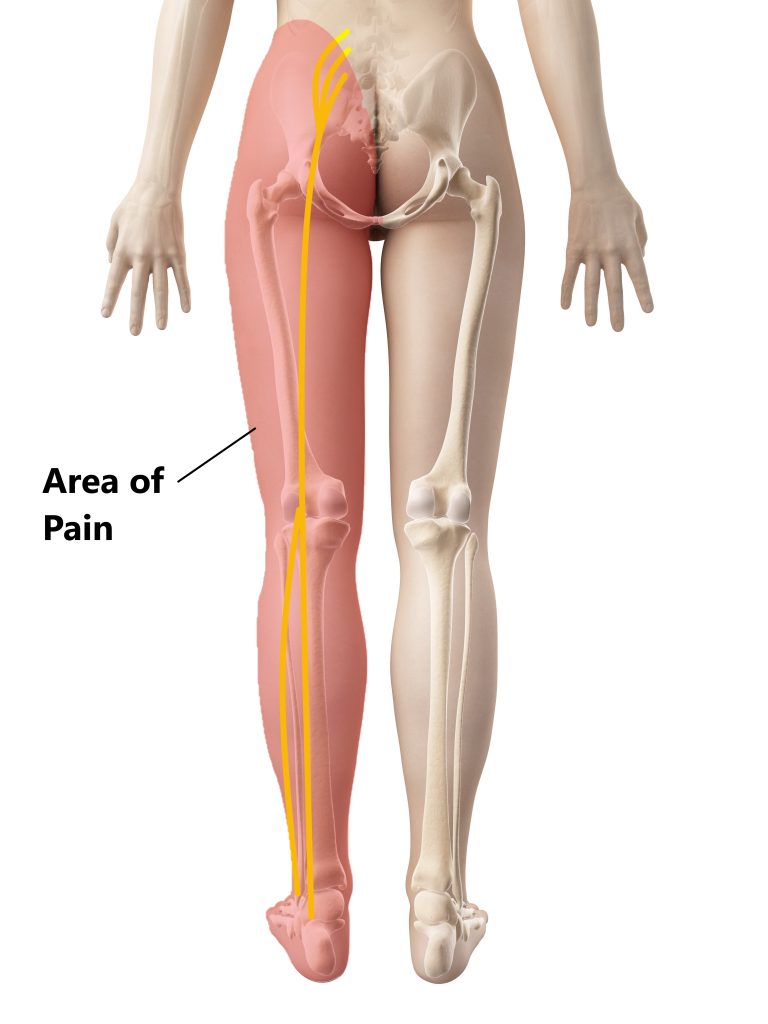
The spinal nerves of the lower back and sacrum merge together and descend into different regions of the leg.
What is the Sciatic Nerve?
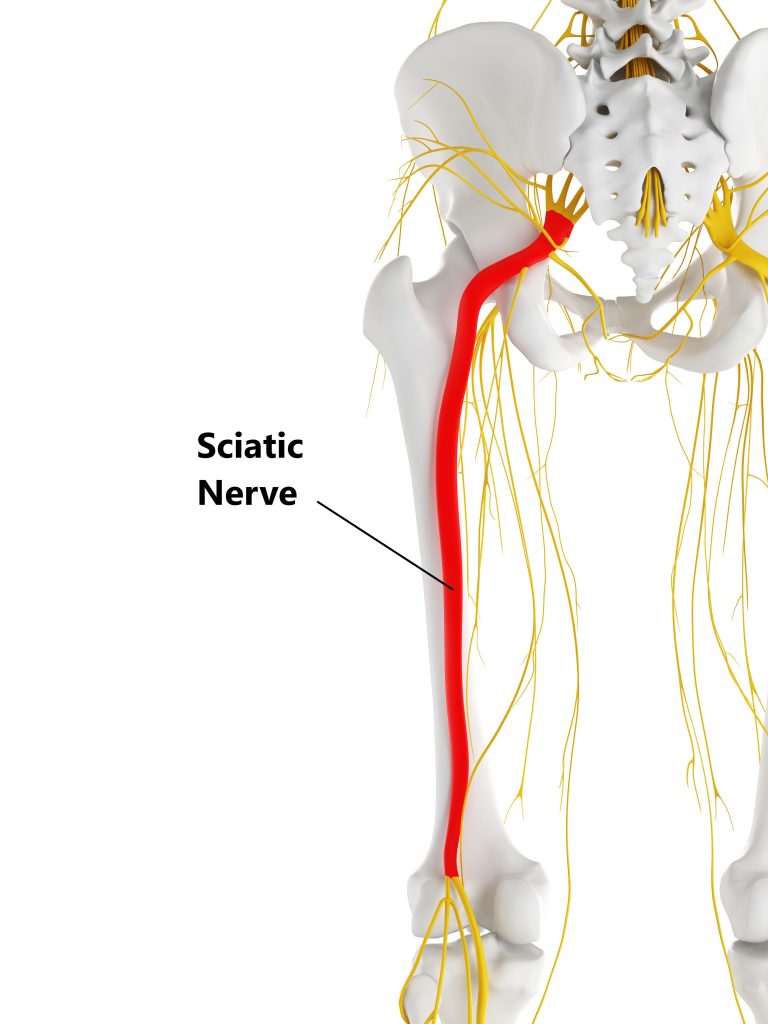
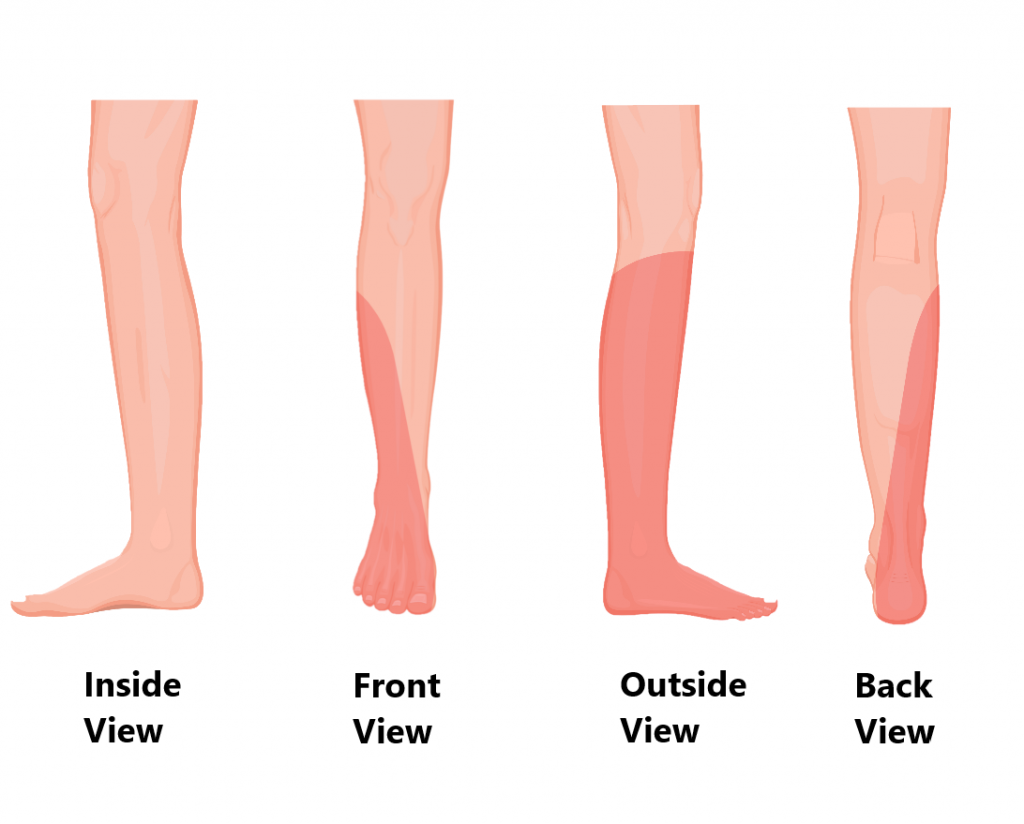
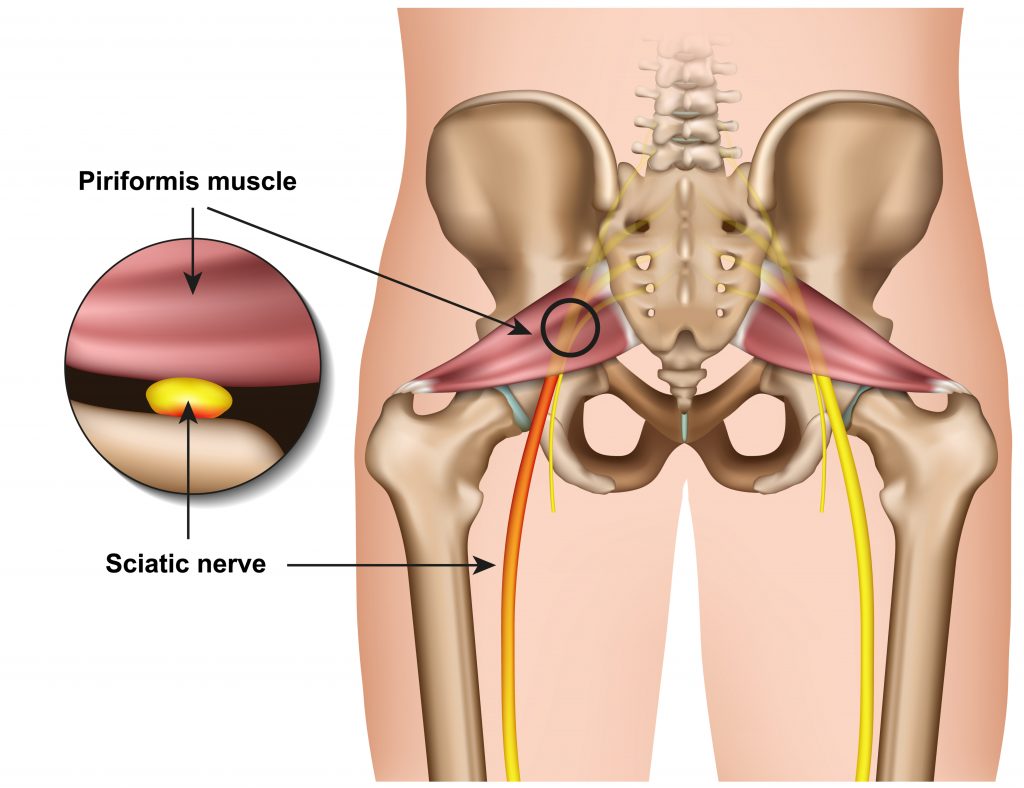
Your sciatic nerve is the largest nerve in the human body and runs down the back of your leg. It travels through your buttock and hamstrings muscles then splits behind the knee to supply the front and back of your lower leg and foot.
What Does Your Sciatic Nerve Do?
Supplies the muscles of the leg to enable movement.
- Bending the knee
- Bringing the leg towards the mid line

- Ankle movement

- Toe movement

Supplies the skin of the lower leg and foot to allow sensation.
What is Sciatica?
“Sciatica” refers to irritation of the nerve as it exits the spine and descends into the foot. This can be due to a physical compression of the nerve tissue or chemical irritation from inflammation. Studies have estimated 13-40% of the population will be affected at some point in their lifetimes.
What Causes Sciatica?
Injuries to the Spinal Structures
Damage to the spinal structures at the L4/5 and L5/S1 levels can cause compression of the spinal nerves or spinal cord and give rise to sciatica.
- IVD Bulge, damage to the outer wall of an IVD can deform its shape causing it to bulge out and compress the spinal nerves or spinal cord.
- Loss of IVD Height, as we age our IVDs begin to loose their water content. This causes a loss of disc height and narrowing of the hole where the spinal nerves exit the spine.
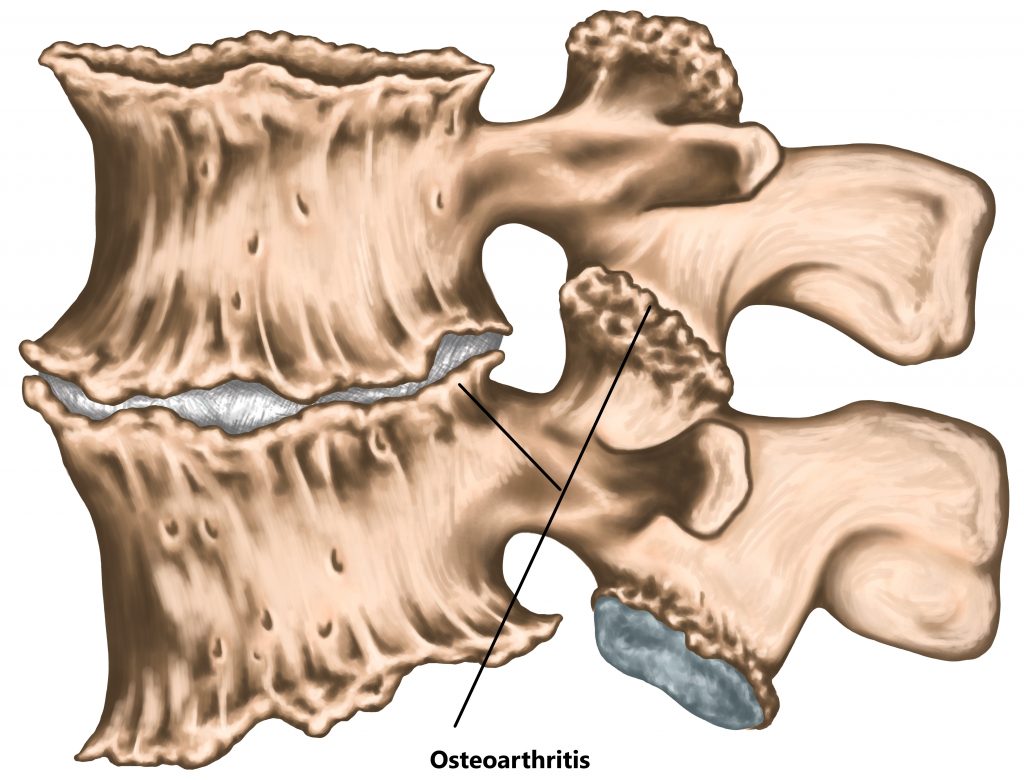
- Osteo Arthritis (OA), advanced OA of the joints in the lower back can result in excessive bone growth and compression of the spinal nerves or spinal cord.
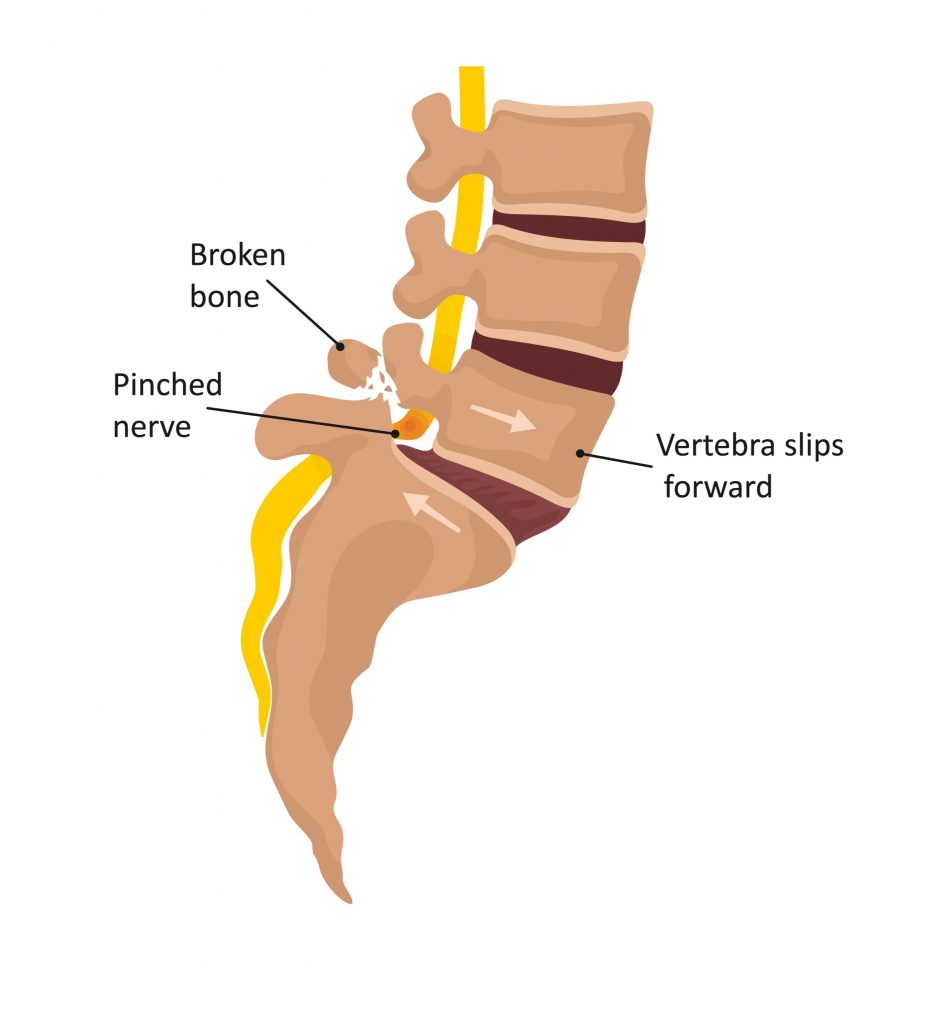
- Joint Instability, advanced wear of the joints in the lower back or stress fractures to the surrounding bone can result in a vertebra slipping forwards or backwards relative to the other segments. This can cause compression of the spinal nerves or spinal cord.
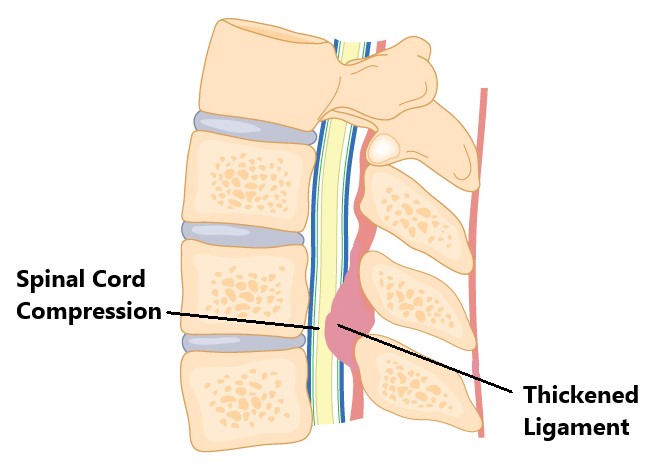
- Calcification and Thickening of Ligaments, this can occur in the ligaments running down the back of the spine causing compression of the spinal cord. This is typically seen in older individuals.
Muscular Causes
- Piriformis, in the buttock region, your sciatic nerve runs very close to your piriformis muscle. Piriformis injuries or excessive tightness can irritate your sciatic nerve.
- Hamstrings, at the back of your thigh your sciatic nerve runs through your hamstrings muscles. Hamstrings injuries or excessive tightness can irritate your sciatic nerve.

Lack of Neural Flexibility
As your sciatic nerve descends down to your foot it travels through many structures (i.e. joints, muscles) and needs to be very flexible. Symptoms can arise if the nerve does not move properly through the bodies tissues.

Inflammation
Inflammation brings chemicals to an injured area which makes you more sensitive to pain. Injuries or infections to surrounding structures (i.e. muscles, tendons, joints, ligaments, IVD) can give rise to excessive inflammation and irritation of the neighbouring nerve tissue.

Pregnancy
During pregnancy your body undergoes several physical changes (i.e. weight gain, looser ligaments, postural changes, fluid retention, expansion of the uterus) making you more susceptible to developing sciatica.

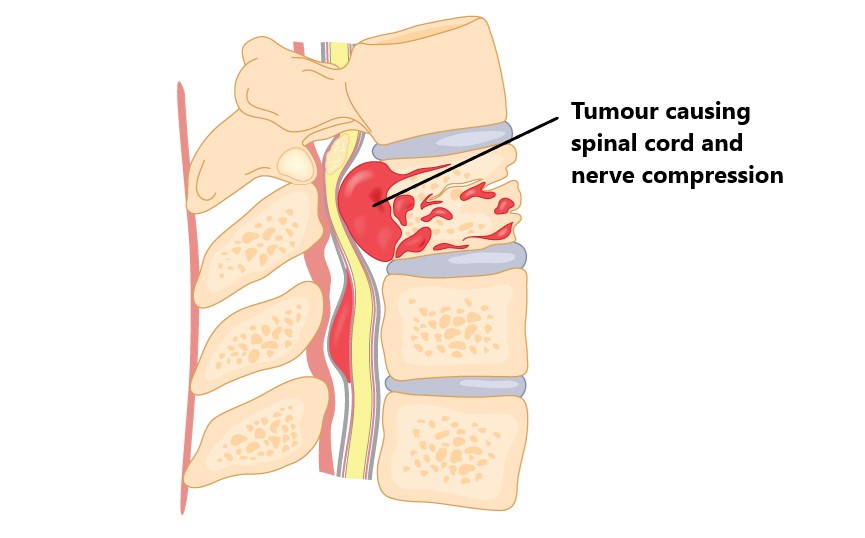
Abnormal Growths
Tumors and cysts can compress the spinal cord or spinal nerves giving rise to sciatica. PLEASE NOTE: Sciatica due to these causes produce constant symptoms that do not change with activity and are also present at night. Please seek urgent medical attention in these situations.
Gynaecological Issues
Referred pain from the lower pelvic area due to gynaecological issues can give rise to sciatica (i.e. ovarian cysts, heavy periods, ectopic endometriosis).
Common Symptoms
- lower back, buttock, posterior leg and foot pain
- numbness
- muscle weakness
- dulled skin sensation in the legs
- hot/cold/burning/electric sensations into legs
- impaired gait
- impaired function
- increased pain with prolonged sitting, bending or walking
- spinal cord compression signs (i.e. loss of bladder and bowel control, increasing clumsiness and weakness in the legs, sudden sexual dysfunction symptoms into both legs). PLEASE NOTE: Urgent medical attention should be sought in these circumstances.

Diagnosis
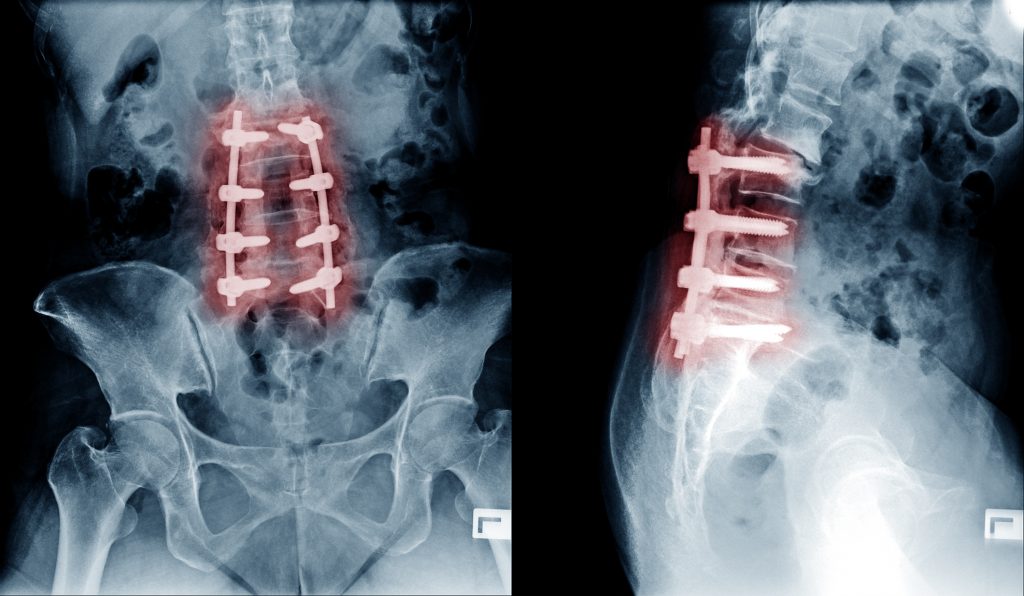
Diagnosing sciatica is mainly based on an individuals clinical presentation through a thorough subjective and physical examination. Imaging may be required to identify the cause of the problem.
- Xray
- CT
- MRI

Risk Factors
- sedentary lifestyle
- lack of physical exercise
- smoking and excessive alcohol intake
- high BMI
- stress, anxiety and depression
- physically demanding occupations
- older age

Management
Sciatica due to musculo-skeletal causes is typically managed with conservative physiotherapy treatment. Thankfully, most cases will resolve within 4-6 weeks of the initial injury. Persistent symptoms may require a cortisone injection to help alleviate symptoms.
Surgery may be considered in rare circumstances where there a is physical compression of the neural structures and a progression of neural signs (i.e. increasing leg weakness, reflex changes, muscle atrophy).
Physiotherapy Management
- Following an acute injury our priority is to minimise the extent of damage, reduce inflammation and decrease pain. Modalities such as modified rest, strapping, manual therapy and acupuncture may be used.
- Provide education regarding the injury, address unhelpful beliefs, identify and modify aggravating factors
- Restore pain free range of motion and return to basic activities. Commence gentle stretches and a walking program
- Restore strength of the core and lower limbs. Commence a graded strengthening program.
- Improved nerve flexibility. Commence specific nerve stretching exercises.
- Identify and address aggravating factors, movement and postural issues that may have contributed to the injury.
- Graded return to work, sport and function.

Red Flags!
These are signs and symptoms of more serious causes and require urgent medical review:
- spinal cord signs (as above)
- symptoms that are also associated with a lack of balance and changes in gait pattern
- sudden onset of symptoms following trauma (i.e. fall, car accident)
- If you get also get symptoms at night that does not change with activity (as above)

Please keep in mind the information provided is general in nature and should not be used as a substitute to consult your treating health professional. If you have any specific questions or require assistance with your individual treatment requirements please do not hesitate to contact MyFamily Physio Pittwater Place Shopping Centre in Mona Vale.
Related Articles