Articles Meniscus Injuries
This article outlines simple anatomy, common injuries and management principles to give you a good basic understanding of meniscus injuries.
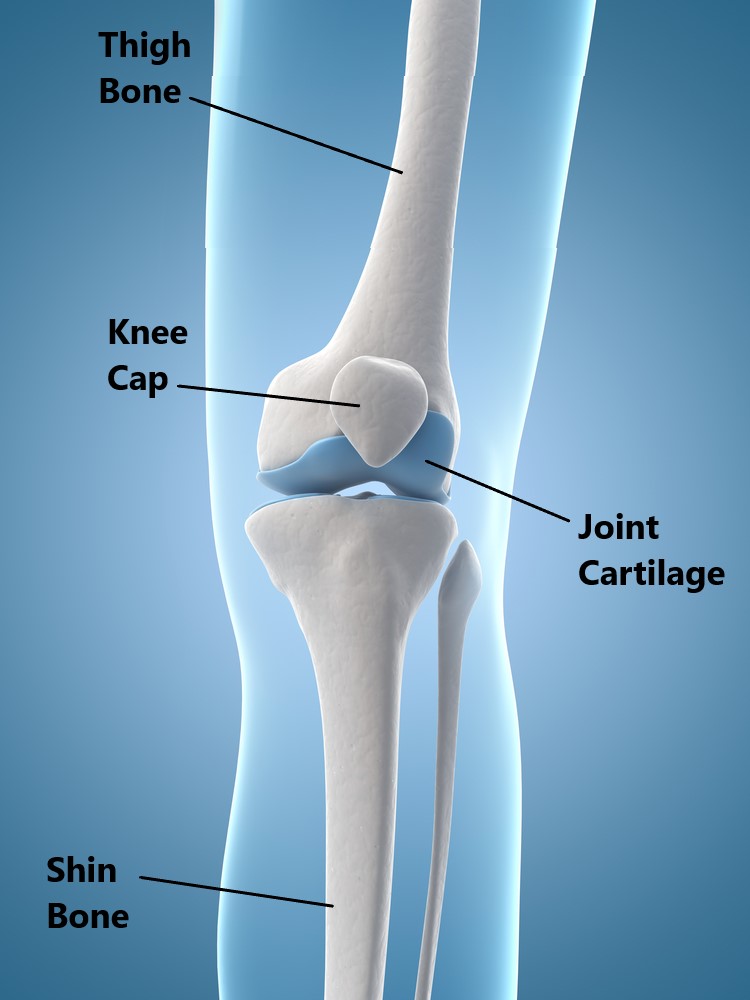
Basic Anatomy
The knee joint is comprised of the knee cap, thigh (femur) and shin bone (tibia). Whenever a bone articulates with another bone there will be a thin layer of joint cartilage. This enables frictionless movement and also provides limited shock absorption.
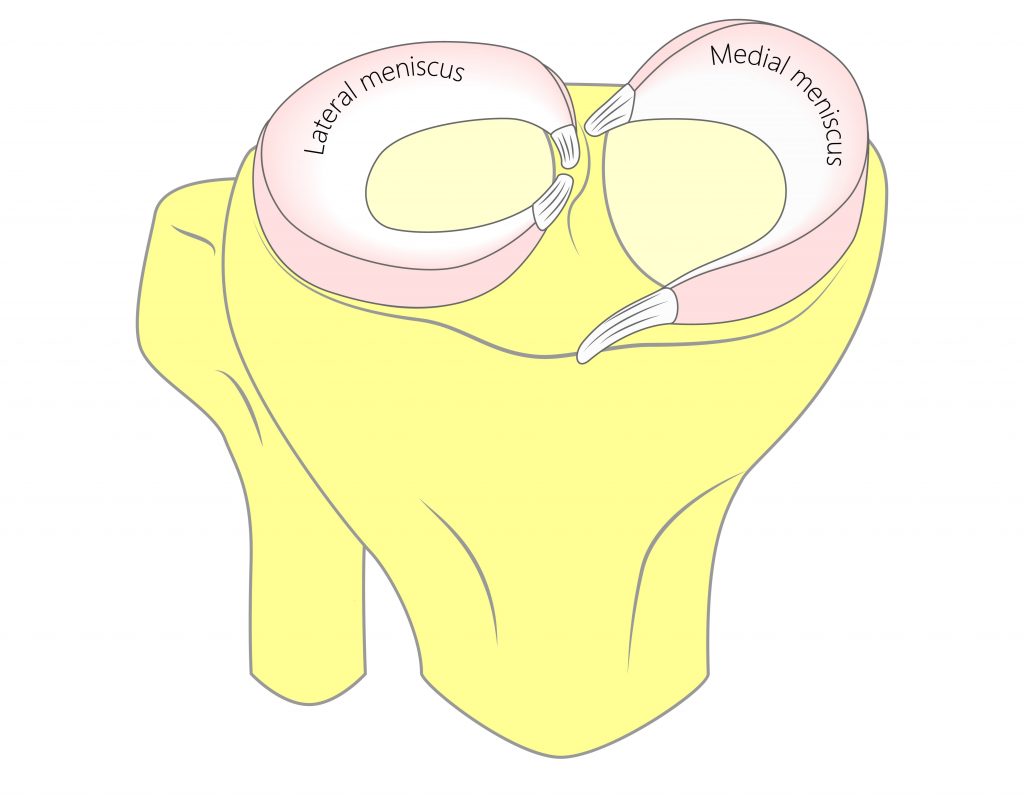
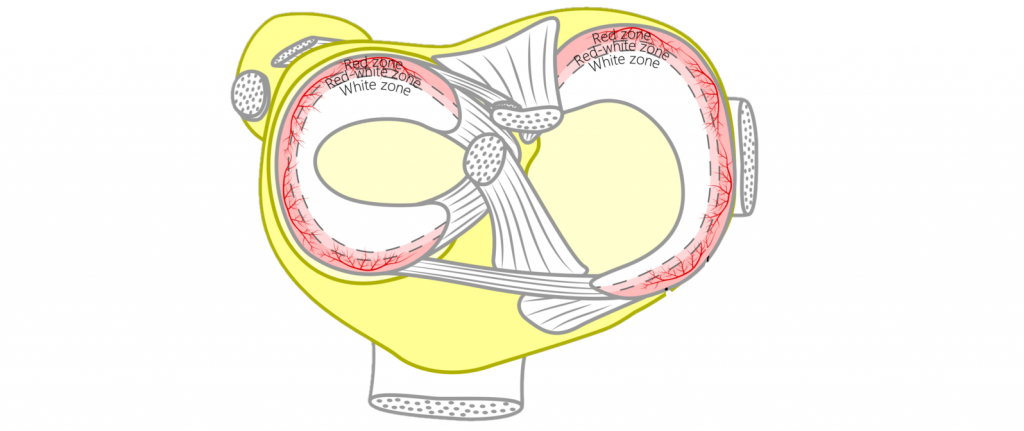
Unique to the knee joint are the additional pads of fibrocartilage located between the femur and tibia. These are known as the lateral and medial meniscus, their primary role is to protect the joint surfaces and absorb shock.
Meniscus Injuries
Meniscus Tears
Meniscus tears are classified according to their location, size and pattern.
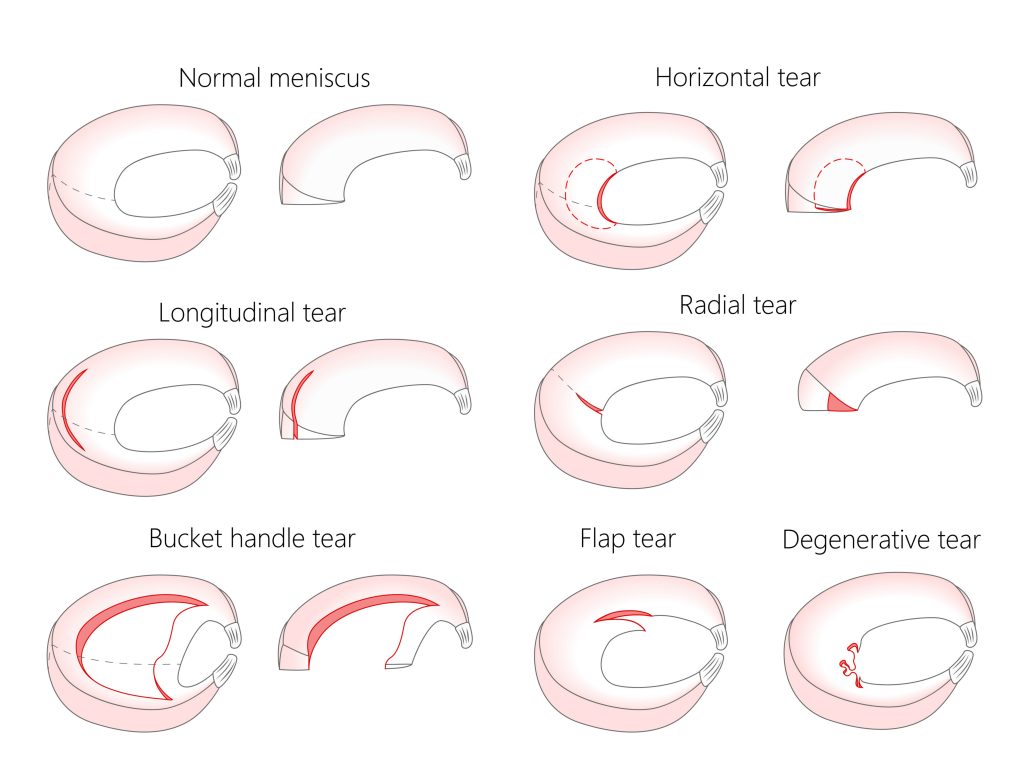
Certain tears have a better chance of recovery than others i.e. smaller stable tears located on the periphery of a meniscus generally heal better than large, unstable centrally positioned tears.
Meniscus tears can be categorised into “acute tears” and “degenerative tears” :
- Acute tears
Acute tears are often seen in athletic populations (i.e. soccer and netball players). A common mechanism of injury typically involves an incident where the individual suddenly pivots all their weight on one foot. Meniscus tears can become more problematic if the torn fragment becomes unstable. This can potentially “jam up” the joint and give rise to symptoms such as locking and giving way of the knee.

- Degenerative tears
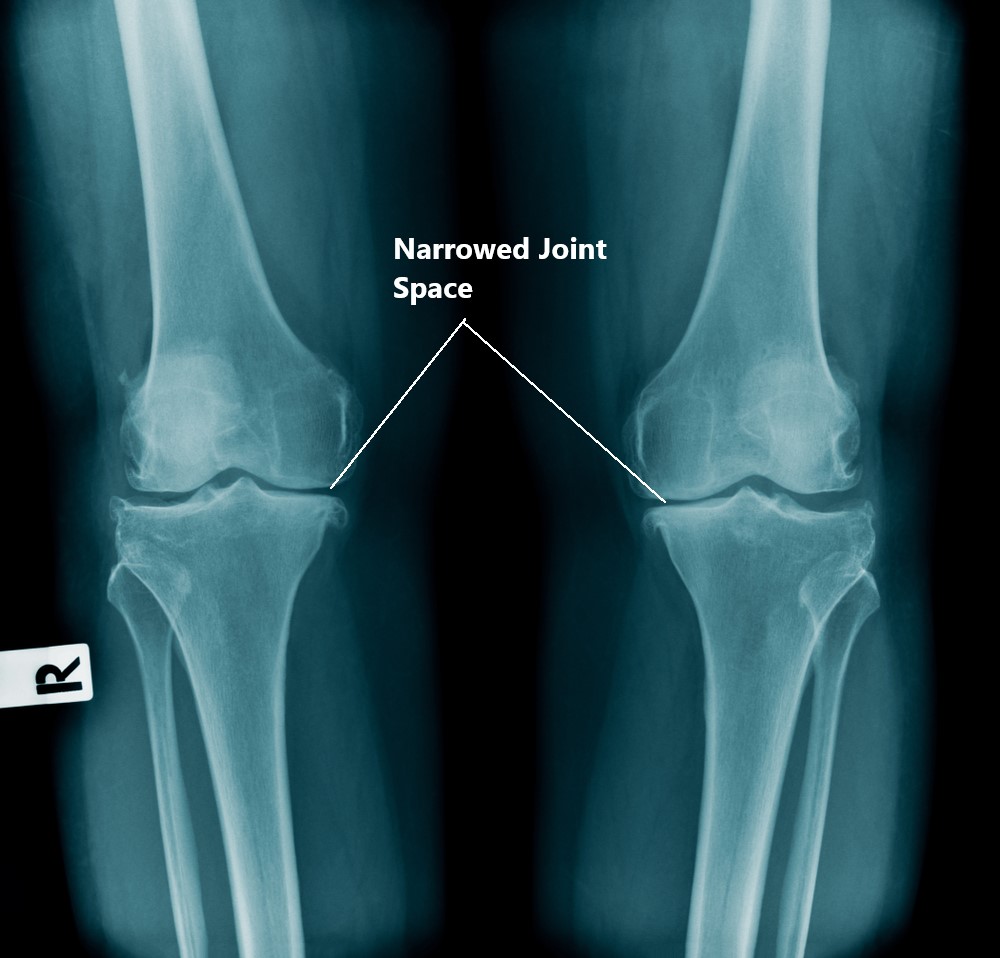
As we age our cartilages naturally loose their water content and become less “springy”, this makes it a lot easier to develop tears (i.e. getting out of a car). Advanced degeneration of the meniscus and joint cartilage will result in bone on bone contact (aka arthritis).
Risk Factors of Meniscus Injuries
- older age
- high BMI
- previous trauma
- engaging in sports involving running and pivoting (i.e. netball, soccer )
- occupations involving prolonged kneeling, squatting and stair climbing
- postural abnormalities of the lower limbs (i.e. being excessively bowlegged or pigeon toed)

Common Symptoms of Meniscus Injuries
- delayed or intermittent swelling
- tenderness along the joint line
- difficulty pivoting on a weight bearing leg (i.e. getting in/out of car, pushing a stubborn shopping trolley)
- lack of confidence walking on uneven ground
- locking of the knee joint
- giving way of the knee
- onset of pain following a single or repeated episodes of weight bearing and pivoting (i.e. changing direction whilst running)

Diagnosis of Meniscus Injuries
Diagnosing a meniscus injury is based on an individuals clinical presentation and imaging. In many cases imaging is not always necessary.
- Subjective examination
- Physical examination
- Xray
- MRI
Other Associated Injuries
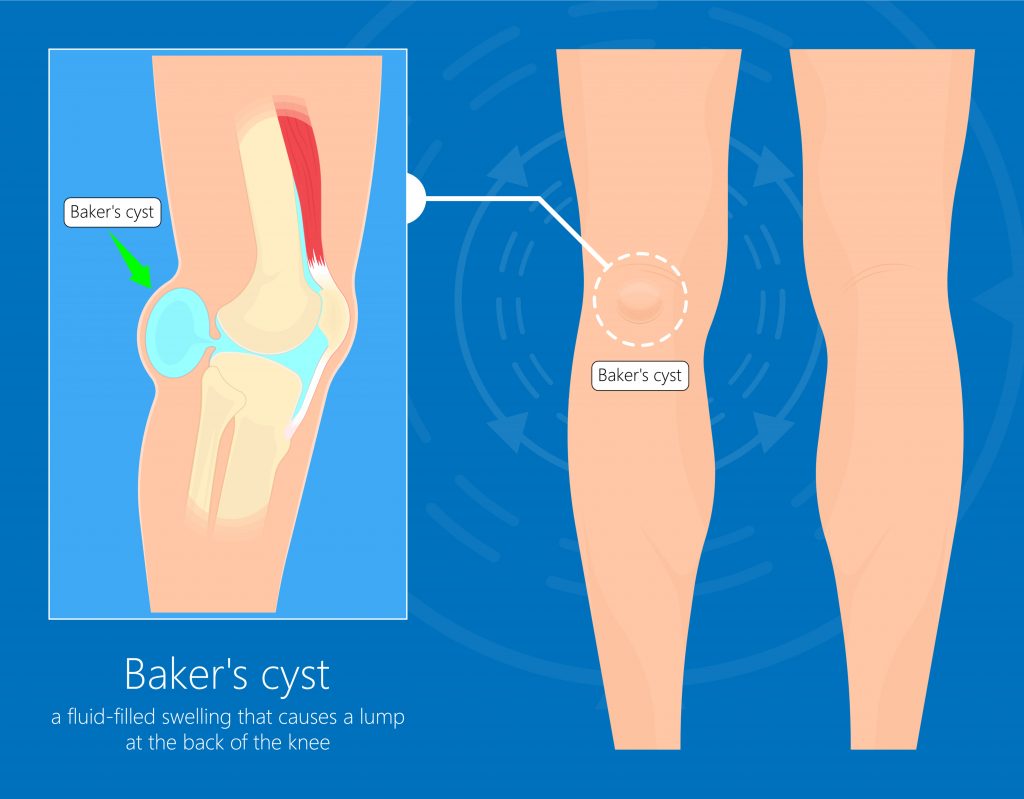
Quite often meniscus injuries do not occur in isolation. Other commonly associated injuries include:
- Ligament injuries (i.e. ACL and MCL tears)
- Osteoarthritis
- Bakers Cyst
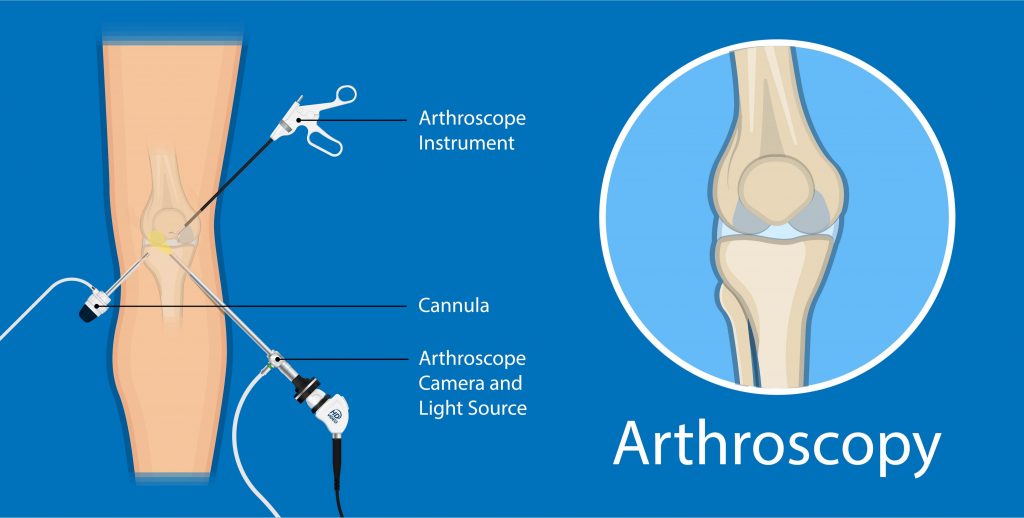
Management
Most meniscus injuries are best managed with conservative physiotherapy treatment. Occasionally, surgery is required to remove unstable fragments and “smooth out” rough joint surfaces (i.e. arthroscopy).
Therapies involving stem cells, donor tissue, cell transplantation and surgical intervention to stimulate repair have shown some promising results but the art of artificially regenerating cartilage has not yet been perfected. ….hopefully this will be available in the near future!
Physiotherapy Management
- Following an acute injury our priority is to minimise the extent of damage, reduce inflammation and decrease pain. Modalities such as RICE (Rest, Ice, Compression, Elevation), strapping and manual therapy may be used.
- Provide education regarding the injury, address unhelpful beliefs and identify and modify aggravating factors.
- Restore pain free knee range of motion and prevent secondary complications (i.e. secondary weight gain, calf shortening)
- Strengthen particularly the VMO muscle and other muscles surrounding the knee joint.
- Identify and address movement and postural issues that may have contributed to the injury (i.e. excessively flat feet, weak hip muscles).
- Graded return to work, sport and function.

Please keep in mind the information provided is general in nature and should not be used as a substitute to consult your treating health professional. If you have any specific questions or require assistance with your individual treatment requirements please do not hesitate to contact My Family Physio, Mona Vale.
Related Articles