Articles Medial Collateral Ligament (MCL) Injuries
This articles discusses basic anatomy of the MCL, functions, causes of injury, symptoms and physiotherapy management.
Basic Anatomy
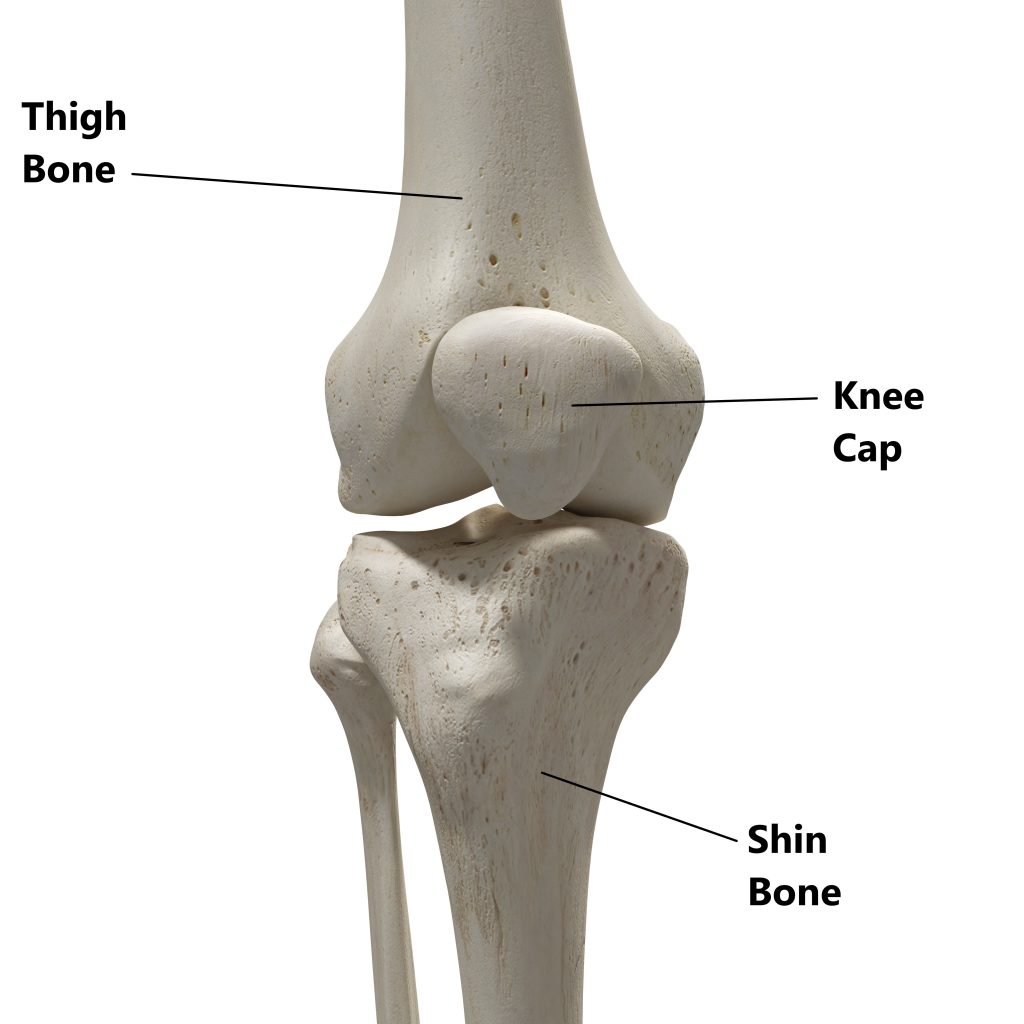
Your knee joint is comprised of 3 bones:
- thigh bone (femur)
- shin bone (tibia)
- knee cap (patella)
Connecting your bones together are the ligaments. These tough fibrous bands of tissue are designed to withstand tension and prevent excessive joint movement. There are 4 major stabilising ligaments in the knee joint:
- Anterior Cruciate Ligament (ACL)
- Posterior Cruciate Ligament (PCL)
- Lateral Collateral Ligament (LCL)
- Medial Collateral Ligament (MCL)
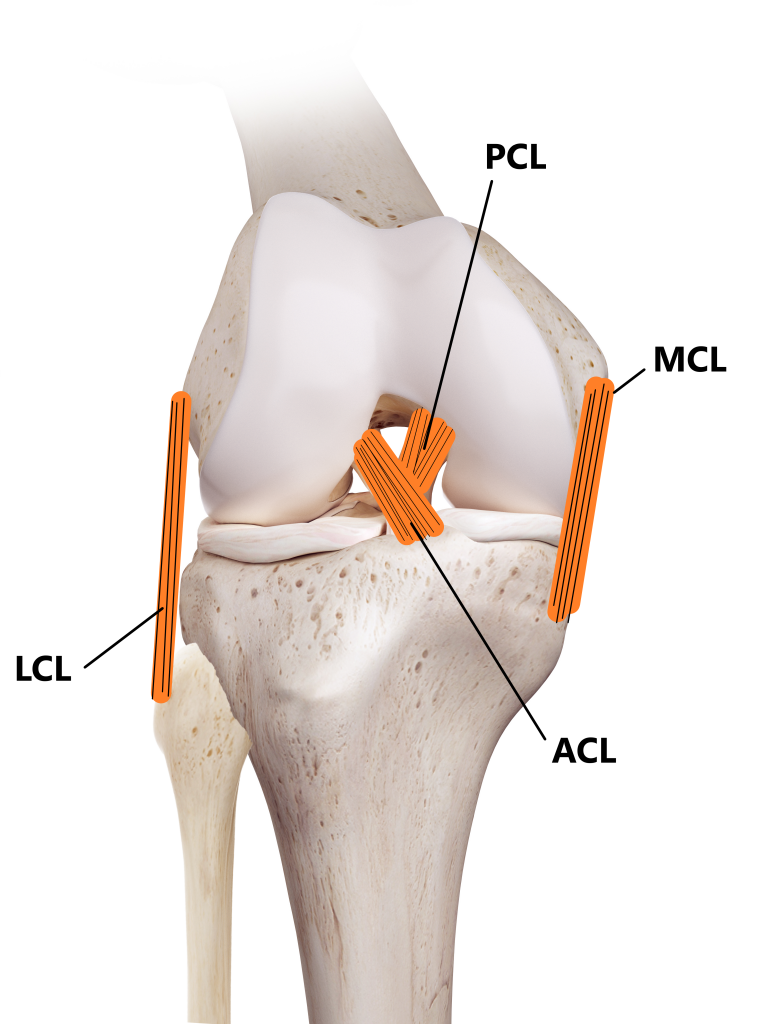
Major ligaments of the knee
Where is Your MCL?
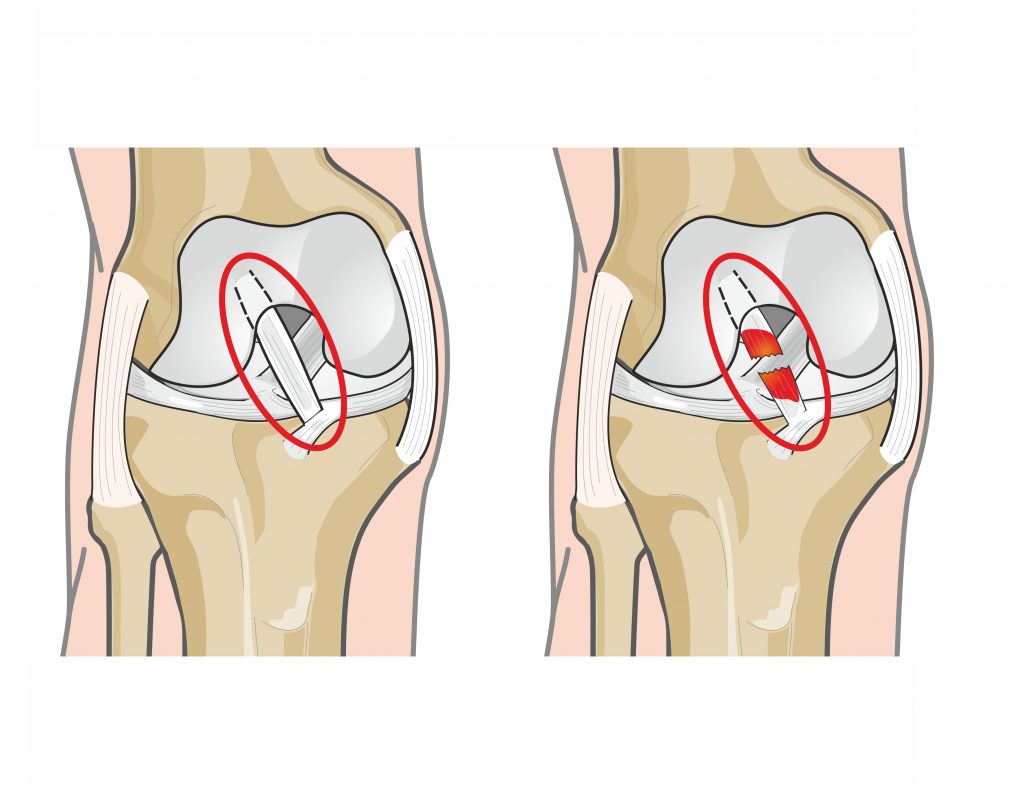
Your MCL is located on the inner side of your knee and connects your thigh and shin bones together. The deeper portions of your MCL also attach to the edge of a cartilage disc (medial meniscus) situated inside the knee joint.
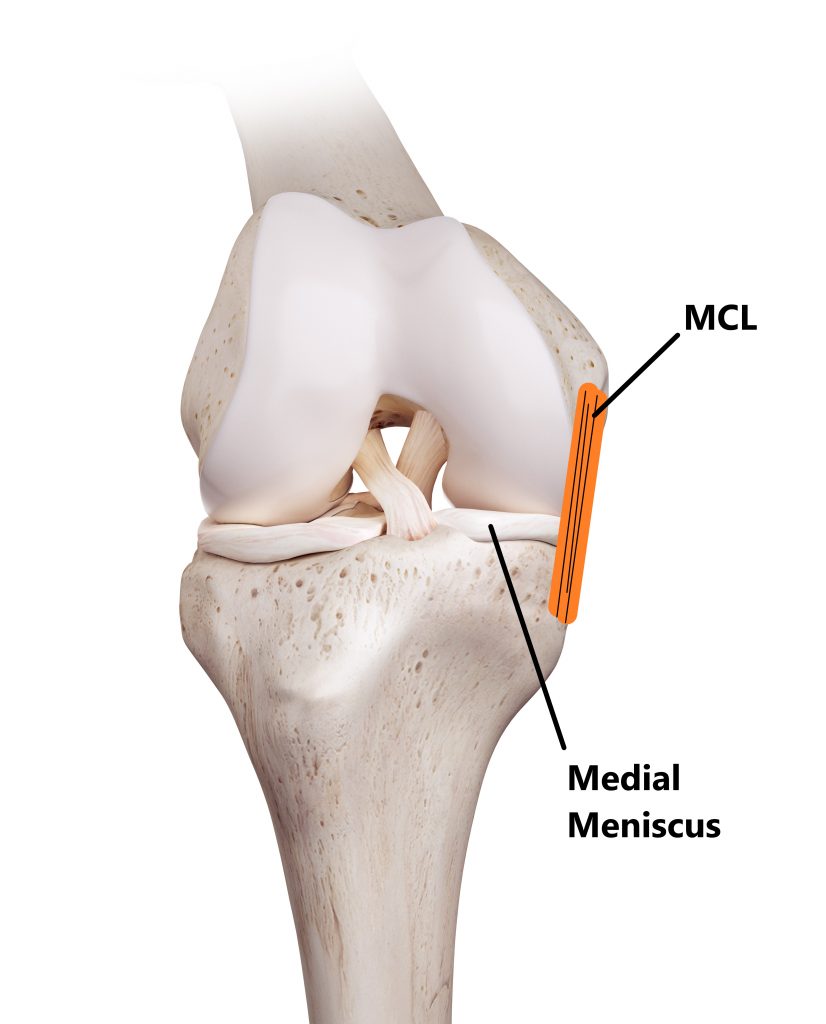
MCL and Medial Meniscus injuries often occur together as the structures are connected
What does the MCL Do?
- The main role of your MCL is to restrict excessive sideways motion between the shin and thigh bone.
- Your MCL plays a role in restricting hyper extension and excessive rotation at the knee joint.

- Nerves inside your MCL help to enhance your sense of balance and leg control.

MCL Injuries
Approximately 40% of all knee ligament injuries involve the MCL making them the most commonly injured. Unfortunately, ligaments have a poor blood supply and are not good at healing. Small sprains take at least 6 weeks to heal and larger sprains can take several months. Sprains can be graded from 1-3:
- Grade 1 mild, micro trauma, minimal loss of range of movement (ROM), minimal swelling, reasonable strength and function, no joint instability
- Grade 2 moderate, partial tear, moderate loss of ROM, delayed moderate swelling, poor strength and function, slight joint instability
- Grade 3 severe, complete/near complete tear, severe loss of ROM, very poor strength and function, significant joint instability (will require an orthopaedic opinion), high likely hood of damage to other structures (i.e. meniscus, ACL)

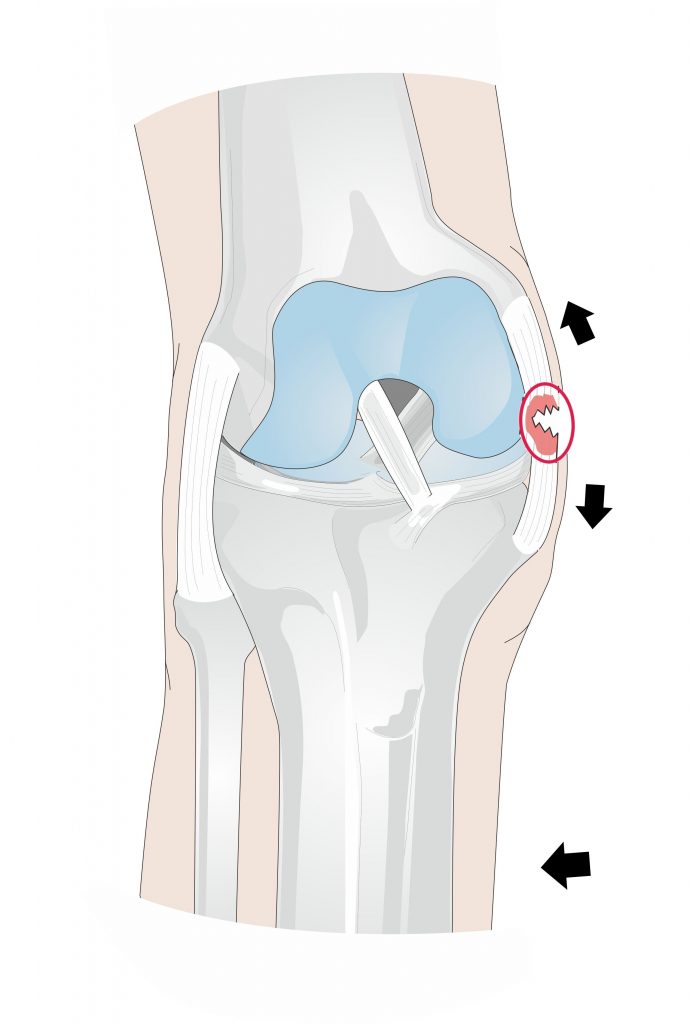
Causes
Acute Trauma, MCL injuries normally involve some kind of acute truama, common mechanisms of injury involve:
- suddenly pivoting inwards on the knee while to foot is planted

- following a blow to the outside of the knee while the foot is planted

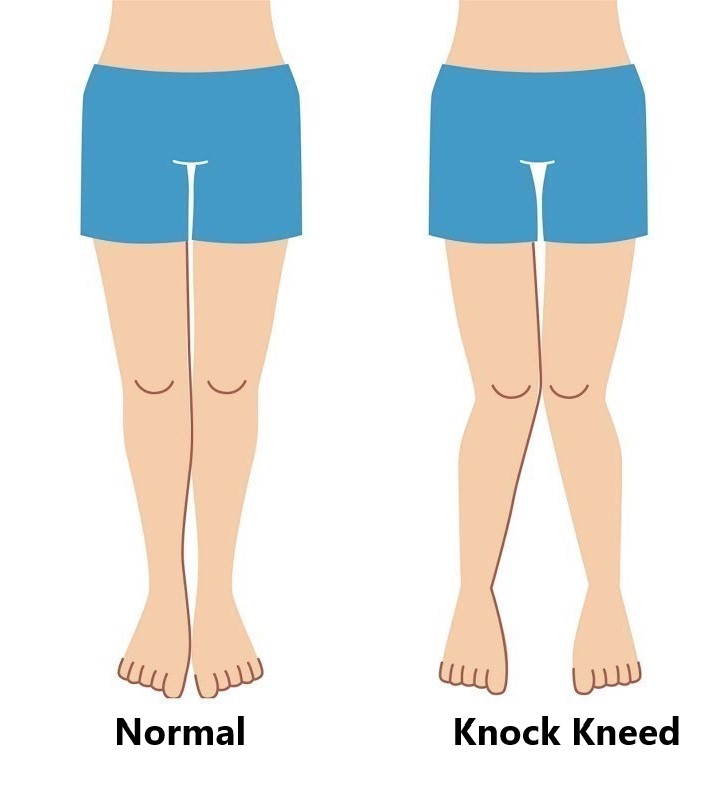
Overuse, repeated overloading of the MCL can eventually give rise to sprains (i.e. knock kneed posture)
Common Symptoms
- hearing a “pop” at the time of injury
- gradual swelling
- pain over the inner side of the knee joint
- instability with weight bearing, especially with pivoting, turning and walking on uneven ground

Diagnosis
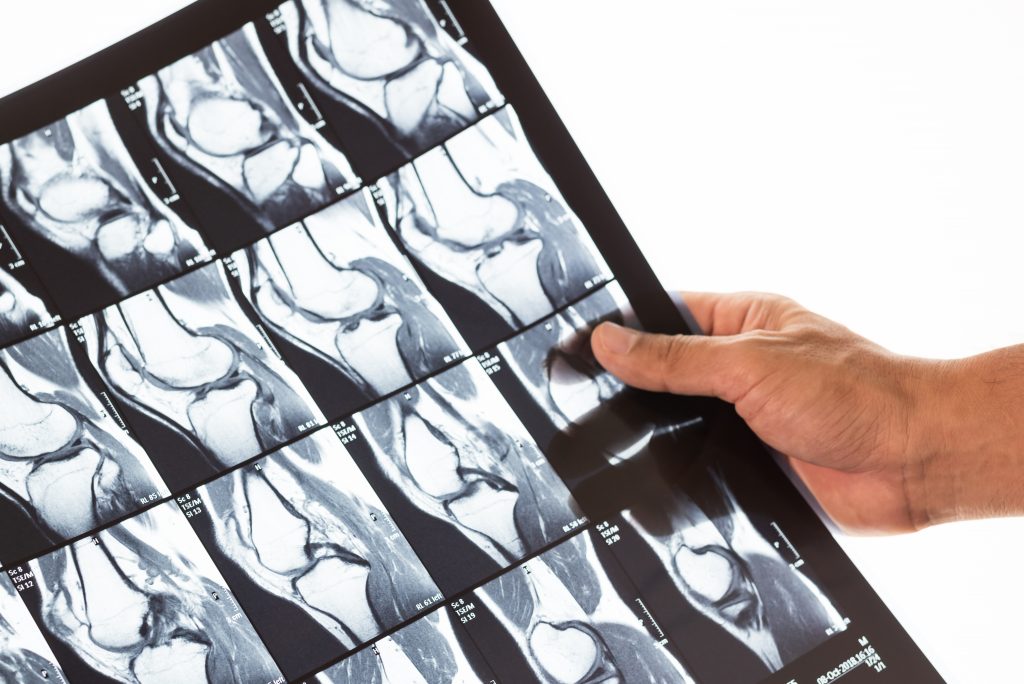
Diagnosing an MCL injury is mainly based on an individual’s clinical presentation through a thorough subjective and physical examination. An Xray and/or MRI may be required for grade 2 and 3 sprains to exclude/identify other injuries.
Common Associated Injuries
- fractures
- meniscus injury
- anterior cruciate ligament injury
Management
MCL injuries are typically managed conservatively. Grade 2 and 3 sprains may require use of a hinged knee brace for several weeks to further protect the ligament while it heals. Surgery is rare for the treatment of an isolated MCL sprain. However, Grade 3 sprains normally involve damage to the neighbouring structures (as above), this increases your chances of requiring surgery.

Physiotherapy Management
- Following an acute injury our priority is to minimise the extent of damage, reduce inflammation and decrease pain. Modalities such as RICE (Rest, Ice, Compression, Elevation), strapping, bracing and manual therapy may be used.
- Provide education regarding the injury, address unhelpful beliefs and identify and modify aggravating factors.
- Restore pain free knee range of motion and prevent secondary complications (i.e. secondary weight gain, calf shortening)
- Strengthen particularly the VMO muscle and other muscles surrounding the knee joint.
- Regain balance and fine motor control .
- Normalise gait/running pattern.
- Identify and address movement and postural issues that may have contributed to the injury (i.e. excessively flat feet, weak hip muscles).
- Graded return to work, sport and function.

Please keep in mind the information provided is general in nature and should not be used as a substitute to consult your treating health professional. If you have any specific questions or require assistance with your individual treatment requirements please do not hesitate to contact My Family Physio, Sydney.
Related Articles