Articles Patellofemoral Pain Syndrome
This article covers basic anatomy, what patellofemoral pain syndrome is, symptoms, causes, diagnosis, medical and physiotherapy management.
Basic Anatomy
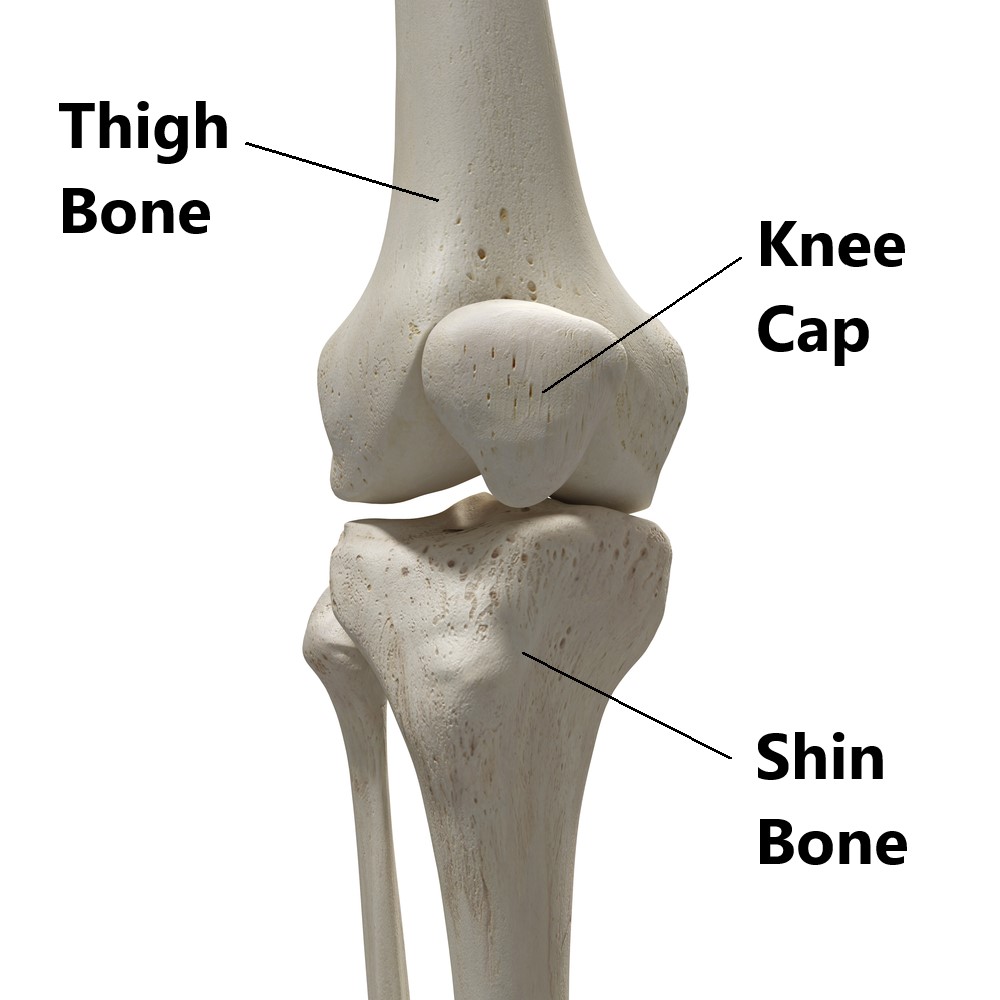
Your knee joint is made up 3 bones:
- Thigh bone
- Shin bone
- Knee cap
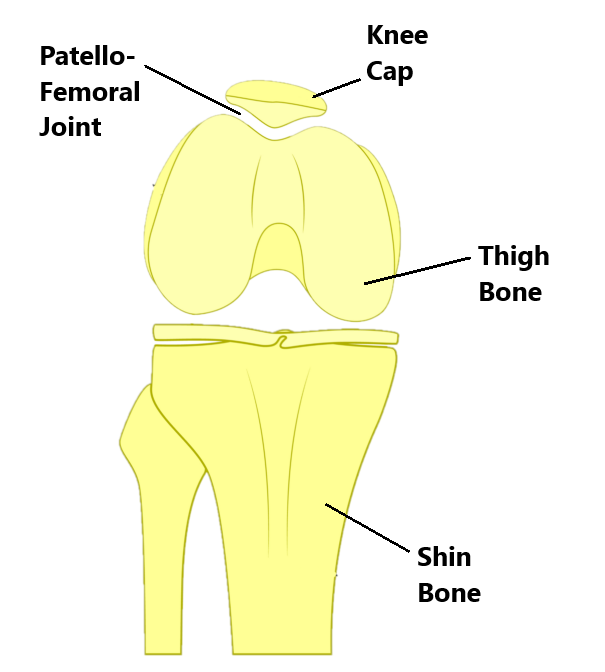
What is the Patellofemoral Joint?
The joint formed between your kneecap and thigh bone is called the patellofemoral joint.
The back surface of your knee cap is “V” shaped. It connects to the front of your thigh bone through a reciprocal “V” shaped groove. As your knee bends and straightens your knee cap should track evenly through this groove.
What is Patellofemoral Pain Syndrome?
This condition refers to pain felt around the knee cap and is one of the most common causes of knee pain.
It occurs when your knee cap becomes misaligned and does not track evenly through the groove in your thigh bone. This can cause rubbing between the bony surfaces giving rise to pain and joint wear.
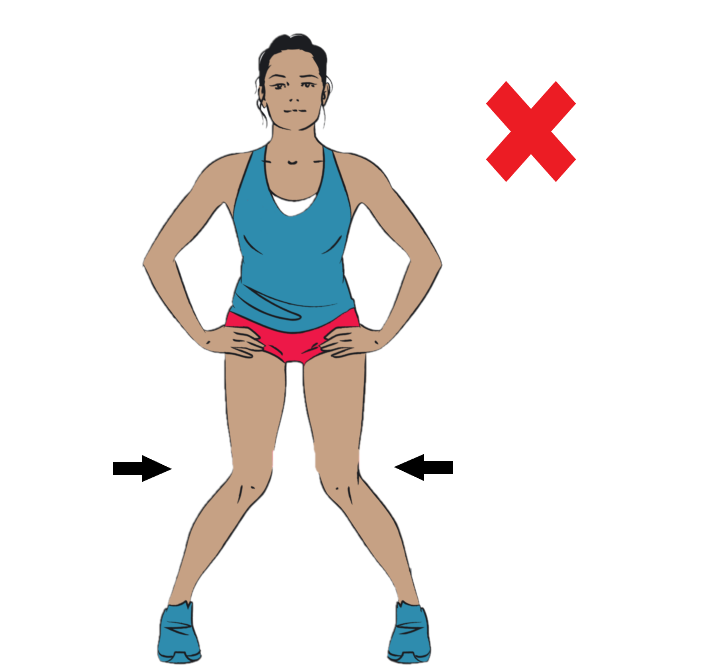
This can happen in different directions however, the most common presentation is where the knee cap drifts to the side away from the midline.
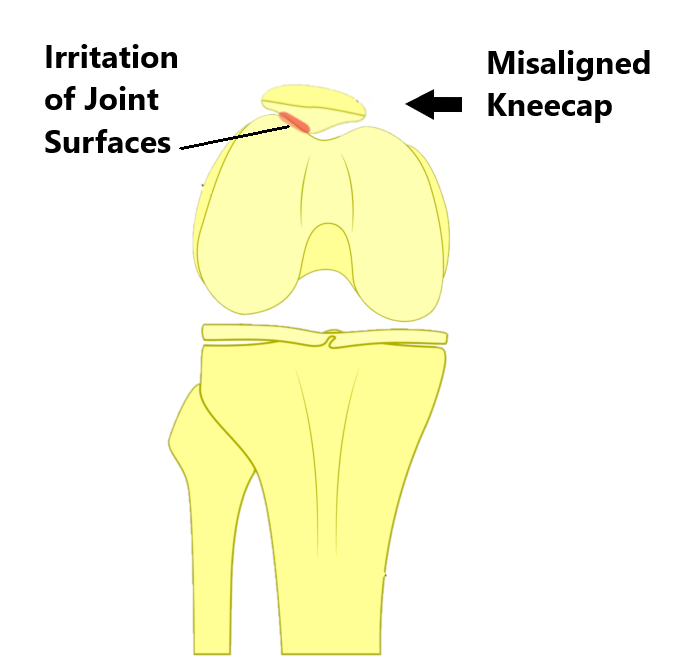
Excessive sideways movement of the knee cap causing rubbing and irritation of the joint surfaces
What Are the Causes of Patellofemoral Pain Syndrome?
Patellofemoral joint pain is often due to multiple factors rather than a single isolated cause. Some common causes include:
- Trauma, Following trauma (i.e. meniscus tear), pain, swelling and inflammation can change how your muscles work around your kneecap. This can make you move unnaturally which places more strain on your patellofemoral joint.

- Overuse, repeated movements such as squatting (i.e. jumping, stairs) and prolonged bent knee positions (i.e. sitting in a chair) can lead to joint irritation.

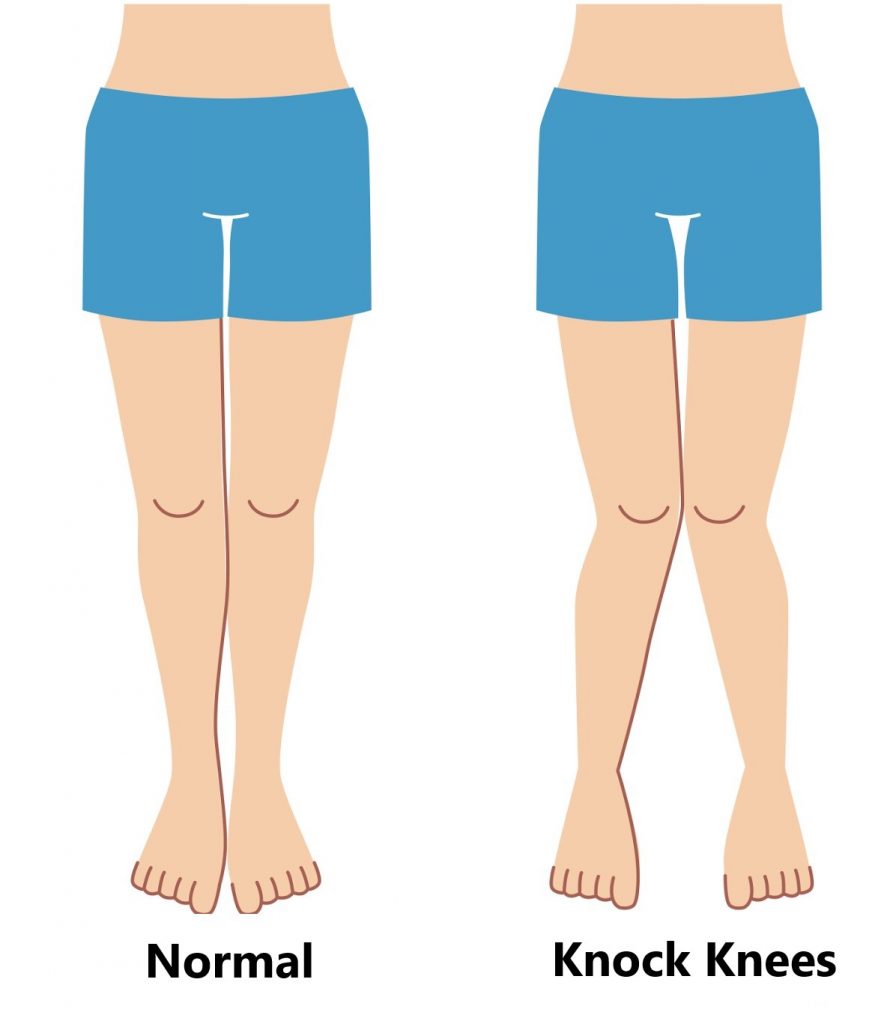
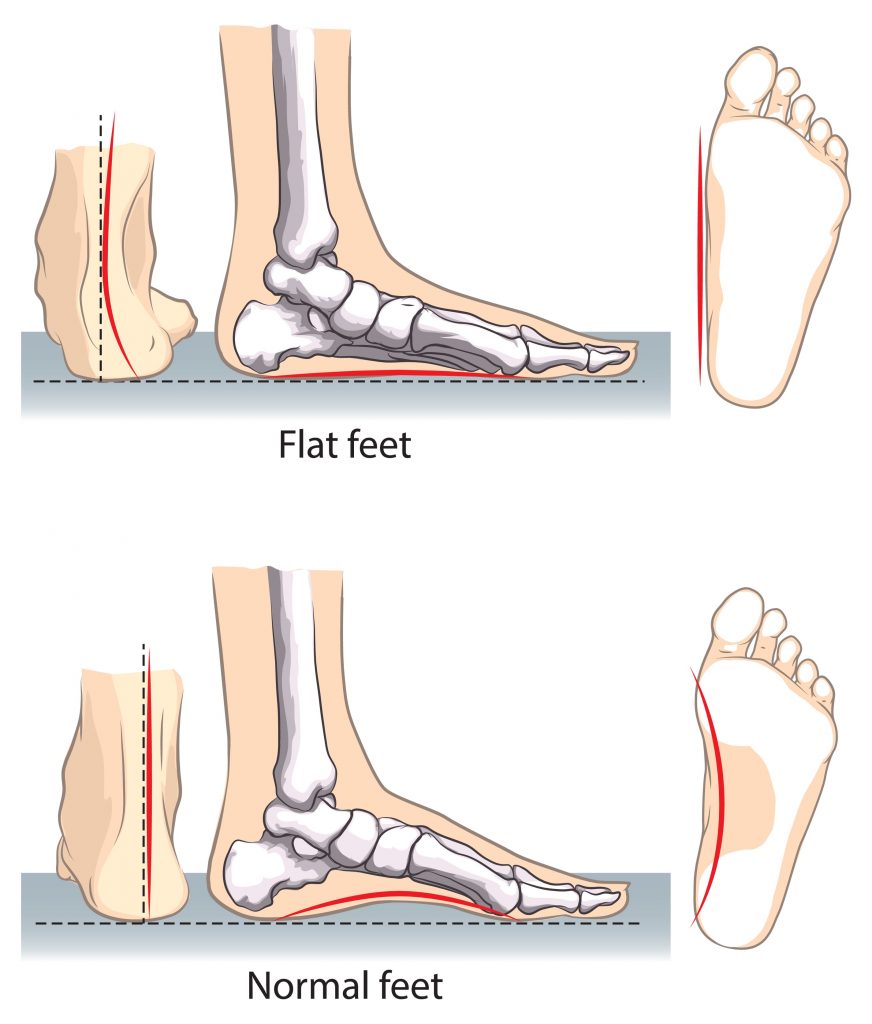
- Poor Leg Posture, this is much like having bad wheel alignment on a car causing uneven wear on the tyres. The most common presentation is a “knock kneed” posture. This is often due to flat feet, weak gluteal muscles and/or poor muscle control.
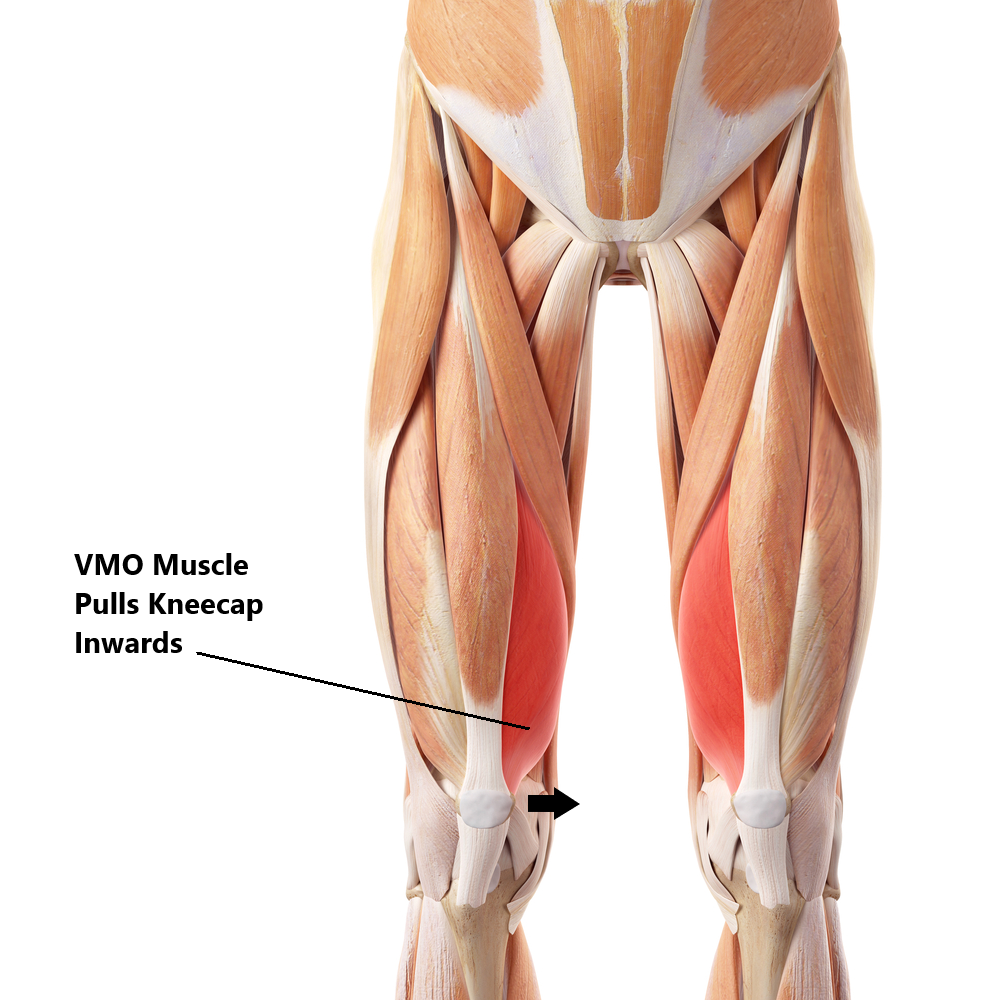
- Weak Vastus Medialus Obliquus (VMO), this is part of your quadriceps muscle and is situated on the inner side of your thigh. It’s job is to stabilise your knee cap in the groove of your thigh bone by pulling it towards the mid line. Excessive weakness can result in your knee cap drifting out towards the side.
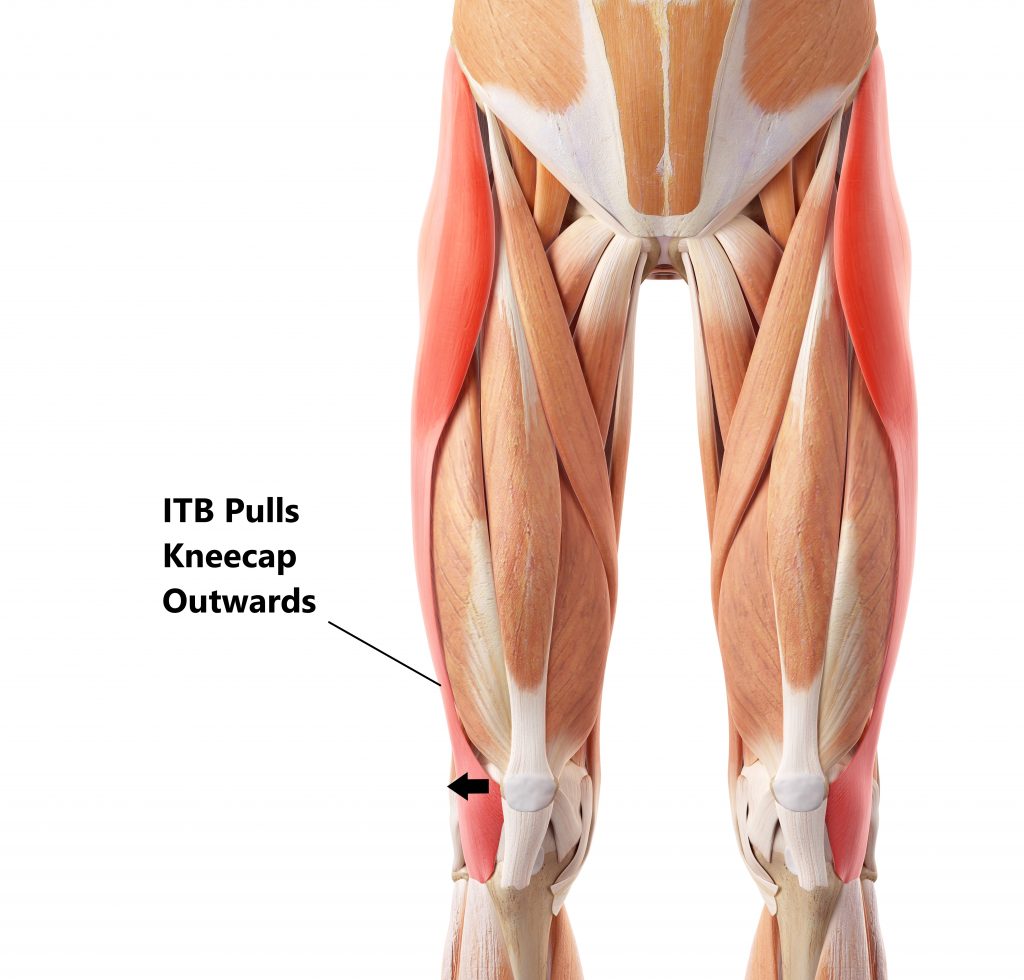
- Tight Iliotibial Band (ITB), this is a long fibrous sheath of tissue situated along the entire length of your thigh. It attaches to structures on the outer side of your kneecap. Excessive tightness can result in the kneecap being pulled out to the side.
- Excessive Muscle Tightness, tight hamstrings and calf muscles can restrict the amount of movement occurring at your hips, knees and ankles. This can place more strain on your patellofemoral joint .

Common Symptoms
- Pain around the kneecap
- Aggravation of symptoms with prolonged sitting, kneeling or squatting
- Aggravation of symptoms ascending/descending stairs
- Aggravation of symptoms with hopping or running

Diagnosis
Diagnosing this condition is mainly based on an individual’s clinical presentation through a thorough subjective and physical examination. An X-Ray or MRI may also be required to exclude/identify other injuries (i.e. Osteoarthritis).

Risk Factors
- History of knee trauma (i.e. patella dislocation)
- Knee surgery (i.e. ACL repair)
- Female gender (this is due females having wider hips which affect knee alignment)
- Participating in running and jumping sports (i.e. basketball)
- Anatomical abnormalities of the legs (i.e. high riding patella, leg length discrepancy, flat feet)
- Individuals with joint hypermobility
Management
Fortunately most cases of PFPS will resolve with conservative physiotherapy treatment (see below). Anti Inflammatory medications and pain killers may help to temporarily relieve symptoms. Surgery is extremely rare for the treatment of this condition.
Physiotherapy Management
- Reduce inflammation and decrease pain. Modalities such as RICE (Rest, Ice, Compression, Elevation), bracing, taping and manual therapy may be used.

- Provide education, identify and modify aggravating factors (i.e. reducing downhill running)

- Restore hip, knee and ankle range of motion

- Strengthening of weak muscles (i.e. VMO, gluteal muscles)

- Correction of lower limb posture (i.e. flat feet, leg length discrepancies)

- Identify and address movement and postural issues that may have contributed to the injury (i.e. poor squatting technique).
Please keep in mind the information provided is general in nature and should not be used as a substitute to consult your treating health professional. If you have any specific questions or require assistance with your individual treatment requirements please do not hesitate to contact My Family Physio in Pittwater Place, Mona Vale.
Related Articles