Articles Plantar Fasciitis
This article covers basic anatomy, what plantar fasciitis is, symptoms, causes, risk factors, diagnosis, medical and physiotherapy management.
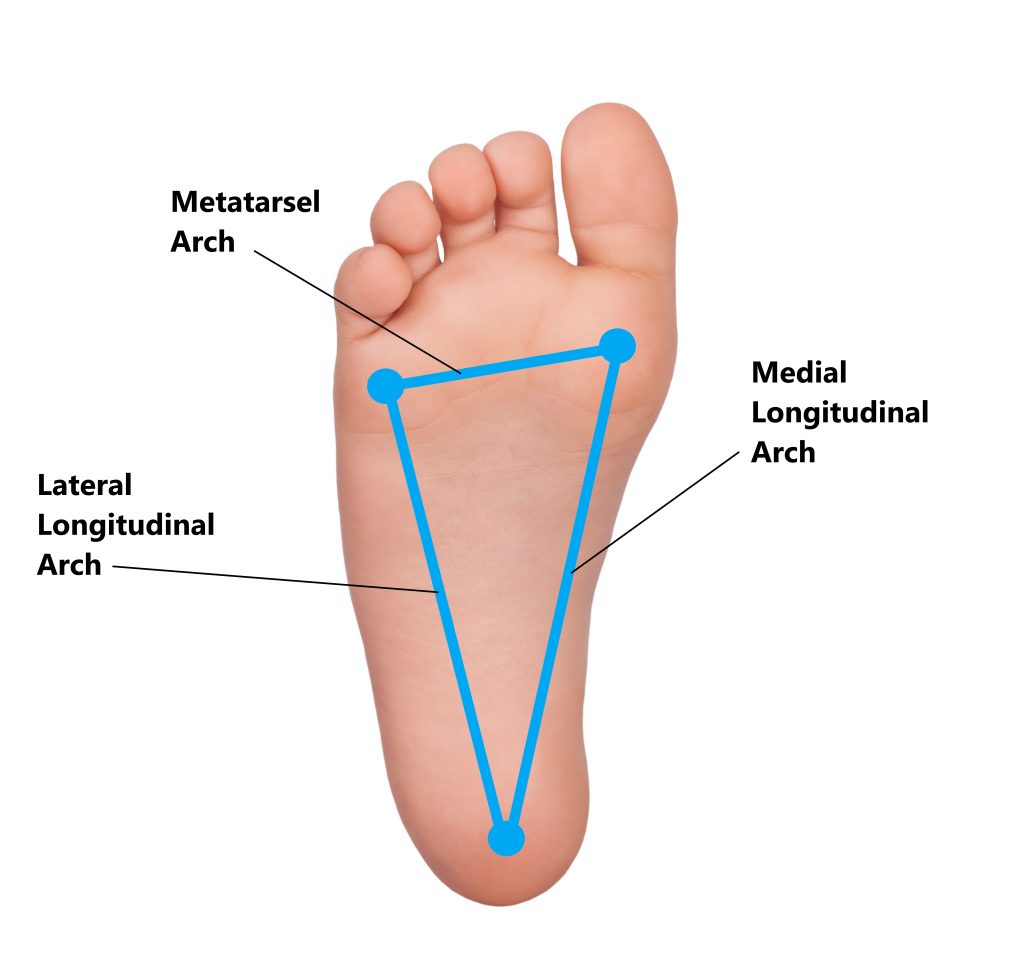
Basic Anatomy
Your foot is a highly complex structure specifically designed for locomotion and weight bearing. The bones of the mid foot are arranged in such a way where arches are formed to help:
- distribute weight evenly
- absorb shock
- propel your forwards as you walk/run
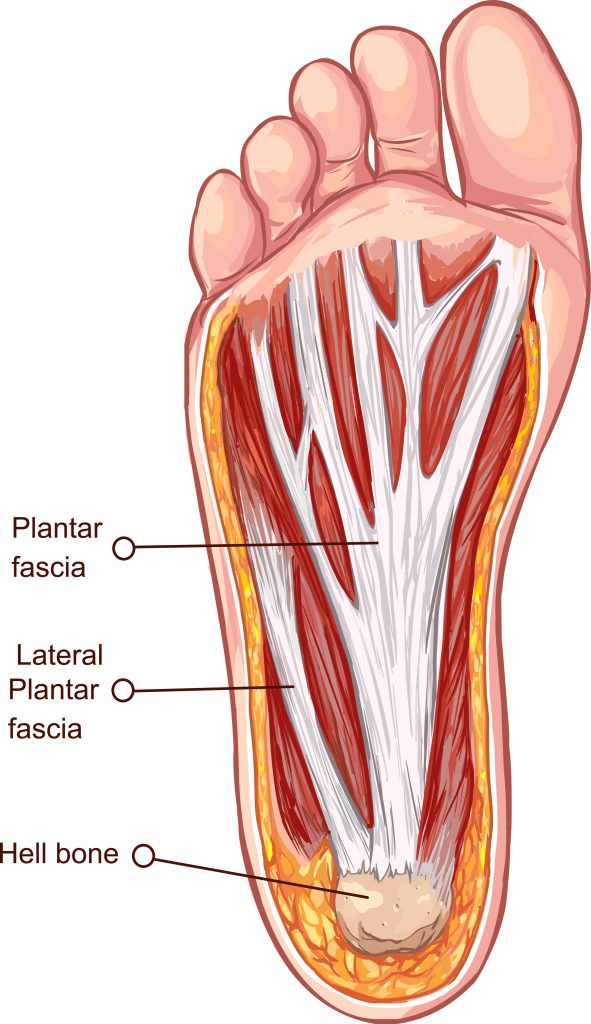
What is the Plantar Fascia?
The plantar fascia is a thick band of tough fibrous tissue located on the sole of your foot. It attaches to the underside of your heel bone and extends towards the base of your toes. This structure assists the muscles, bones and ligaments to support the arches of the foot.
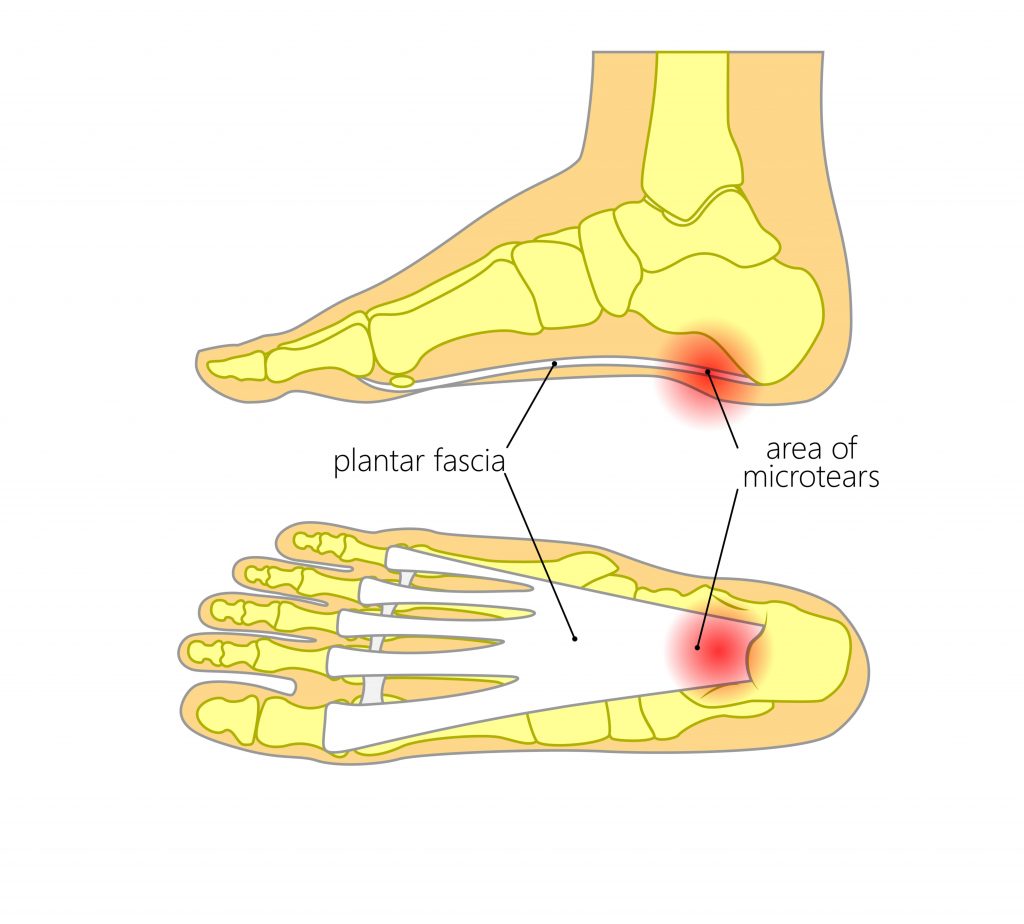
What is Plantar Fasciitis?
Micro tears and inflammation of the plantar fascia can give rise to this condition. This usually occurs where the plantar fascia attaches to the heel bone.
This is most commonly observed in people between the ages of 40-60 years. Unfortunately, an inability to adequately rest the foot will further aggravate the condition and result in prolonged recovery times (i.e. several months). In chronic cases, prolonged inflammation can result in calcification and formation of a heel spur.

Causes
This condition can arise from:
- Overuse (i.e. prolonged standing, excessive walking/running)

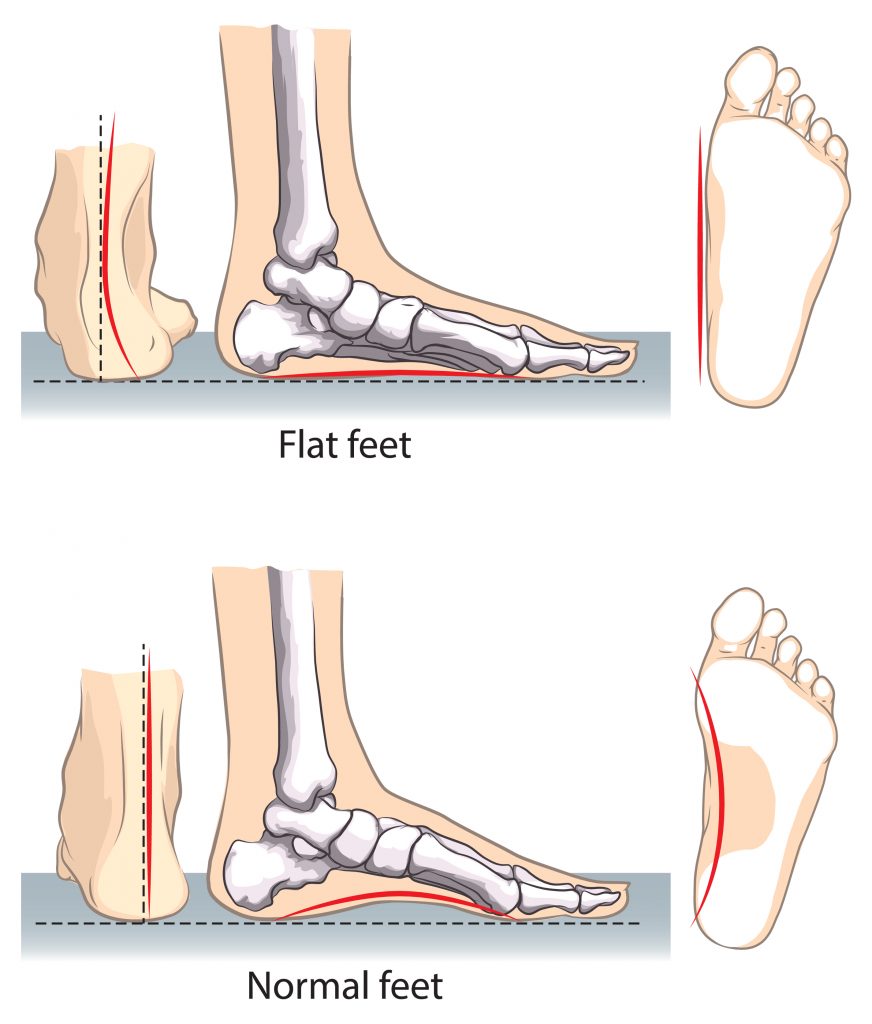
- Over stretching of the plantar fascia (i.e. flat medial foot arches)
- Sudden impact (i.e. landing heavily on your heel)

What are the Symptoms of Plantar Fasciitis?
- Pain along the medial arch/underside of heel bone
- Severe pain with the first few steps following a long period of rest (i.e. first thing in the morning)
- Aggravation of symptoms with prolonged standing, walking or running
- Aggravation of symptoms when weight bearing barefoot
- Aggravation of symptoms when weight bearing on hard surfaces (i.e. wooden floors)

Risk/Contributing Factors
- Excessively high or low medial arches
- Being overweight or sudden weight gain (i.e. pregnancy)
- Occupations involving prolonged standing
- Participating in running sports
- Inadequate footwear
- Excessively tight lower leg muscles
- Stiff ankle joints
- Diabetes

Diagnosis
Diagnosing this condition is mainly based on an individual’s clinical presentation through a thorough subjective and physical examination. An xray, ultrasound or MRI may also be required to exclude/identify other injuries.

Management
- Most cases will recovery with conservative physiotherapy treatment (see below)
- Anti inflammatory medications (i.e. Nurofen)
- More persistent cases may benefit from a cortisone injection into the plantar fascia
- Surgery is rare and only indicated in severe long standing cases where conservative treatment has failed

Physiotherapy Management
- Reduce inflammation and decrease pain. Modalities such as RICE (Rest, Ice, Compression, Elevation), taping and manual therapy may be used

- Provide education, identify and modify aggravating factors

- Exercises to stretch out the affected muscles and increase ankle joint movement

- Strengthening your core, hip and leg muscles to improve your lower limb posture

- Correction of foot wear (i.e. orthotics)

Please keep in mind the information provided is general in nature and should not be used as a substitute to consult your treating health professional. If you have any specific questions or require assistance with your individual treatment requirements please do not hesitate to contact My Family Physio in Pittwater Place Shopping Centre.
Related Articles